Boosting PCOS diagnosis, treating afib, and more stories
This month's issue covers polycystic ovary syndrome, atrial fibrillation, and early career physicians learning how to make referrals.
Although polycystic ovary syndrome (PCOS) may sound like a reproductive disease, its name belies its metabolic underpinnings. In fact, it's the most common endocrine disorder among reproductive-age women, but many, perhaps most, are initially misdiagnosed. In our lead cover story in this issue, Senior Writer Gianna Melillo talks to experts to learn more about PCOS in primary care.
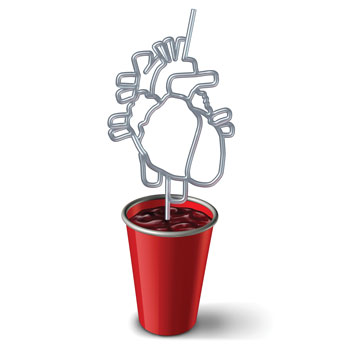
Recently, the American College of Cardiology, American Heart Association, and other professional societies released updated recommendations on atrial fibrillation for the first time in about a decade. Among other changes, the guideline highlights the value of lifestyle changes and recommends earlier use of rhythm control treatments in eligible patients. It also introduces a classification system that divides afib into four stages of progression, rather than focusing solely on arrhythmia duration. Our story offers more details on what's new.
If you're just starting out in your practice, you may feel a little lost when it comes to referrals. Determining the best subspecialist to recommend for a given patient involves building a network and cultivating relationships, but specific requests, timely follow-up, and e-consults can help, too.
Speaking of communication between primary care and subspecialist physicians, this can be particularly difficult when patients with end-stage renal disease begin dialysis. While some dialysis patients are managed entirely by their nephrologists, others continue to see their primary care physicians for comorbid conditions and preventive care, and information doesn't always flow both ways as needed. Nephrologists and primary care physicians should work together to educate patients about what to expect, including medication changes, symptom management, and advance care planning, according to experts.
One way ACP works to support its members is by reviewing and evaluating the validity of existing performance measures in various areas of patient care. The current Chair of ACP's Performance Measurement Committee discusses the College's most recent work on quality measures for major depressive disorder, explains why only one of eight reviewed measures was supported, and outlines what's needed for a quality measure to function as intended.
Also in this issue, a feature story takes you to ACP's annual Leadership Day, held in May, where internal medicine physicians, residents, and students met with members of Congress and their staff to advocate for ACP priorities, including bills to ease administrative burdens, boost the physician workforce, and protect physician payments. And in our Pearls from I.M. Peers column, a women's health expert offers advice on managing patients with low sexual desire and gives her opinion on whether over-the-counter menopause tests are useful (spoiler: usually not).
Do you have a top tip for handling patient referrals, or a clinical pearl to share? Let us know at immatters@acponline.org.
Sincerely,
Jennifer Kearney-Strouse
Executive Editor