Better diagnosis, treatment of PCOS
Up to 70% of women with polycystic ovary syndrome (PCOS) go undiagnosed and one-third experience diagnostic delays of more than two years.
Diabetes and thyroid disease are well-known endocrine disorders, but there's another that tends to receive much less attention, leaving patients frustrated by diagnostic delays and inadequate information.
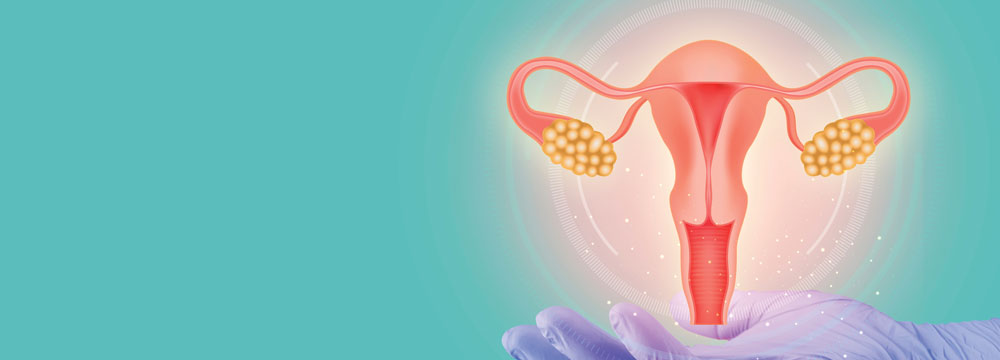
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder affecting reproductive-age women. Between 8% and 13% of women in this age group have PCOS, with some estimates as high as 20%, a total that's “irrespective of ethnicity, irrespective of geographic location,” explained Anuja Dokras, MD, MHCI, PhD, director of the Polycystic Ovary Syndrome Center at the University of Pennsylvania in Philadelphia. “That's huge. That's much more than diabetes and thyroid [disorders].”
However, up to 70% of women with PCOS go undiagnosed, according to June 2023 estimates from the World Health Organization. Around one-third of women with PCOS experience diagnostic delays of over two years, while nearly half see at least three health care professionals before being diagnosed, a 2017 study published by the Journal of Clinical Endocrinology and Metabolism found.
“Patients express that they [are] very disappointed with the diagnosis experience. Many patients go from one physician to another, there's a lot of frustration and disappointment with the diagnostic part, and then with the management and treatment,” said Dr. Dokras.
Clarifying misconceptions
Perhaps the most basic misconception that can contribute to confusion around PCOS is that the condition's title is a misnomer.
“There are no cysts in the ovaries. What [clinicians] see on ultrasound, and used to see on surgery, are follicles, which are the normal structures that contain the oocytes, and as they mature, they have some fluid within the follicle,” said Andrea Dunaif, MD, an internal medicine physician and system chief of the division of endocrinology, diabetes, and bone disease at the Icahn School of Medicine at Mount Sinai in New York. Women with PCOS have more of these follicles, she said.
What's more, the absence of such cysts on ultrasounds is not an exclusion criterion for PCOS, explained Skand Shekhar, MD, MHSc, FACP, an internal medicine physician, endocrinologist, and clinician investigator in endocrinology and reproduction at the National Institute of Environmental Health Sciences in Research Triangle Park, N.C. “As long as some of the other diagnostic criteria are met, it is not even any more necessary to do an ultrasound of the ovaries in adults,” he said.
In 2023, experts, including Dr. Dokras, published updates to international PCOS guidelines that included a consensus on 2003 Rotterdam criteria for diagnosing PCOS. According to the updates, patients must present with at least two of the following features to receive a diagnosis: clinical/biochemical hyperandrogenism, ovulatory dysfunction, or polycystic ovaries on ultrasound or high levels of the anti-Müllerian hormone.
Based on their presentations, patients fall into different PCOS phenotypes that can determine treatment going forward.
For managing the medical consequences of PCOS, you don't need to know anything about what the ovaries look like, Dr. Dunaif reiterated. “You just need to know whether there is evidence for increased male hormone action.”
This evidence includes not only elevated circulating male hormone levels (most frequently levels of free testosterone, which is testosterone that is not bound to sex hormone-binding globulin), but also hirsutism, she said. She noted that some women who have normal circulating male hormone levels can have increased coarse hair growth in male hormone-dependent hair follicles on the face and trunk.
Hirsutism is considered to be a reliable marker for hyperandrogenism, but acne and scalp hair loss are not, so the presence of hirsutism fulfills diagnostic criteria for hyperandrogenism, Dr. Dunaif said. Hyperandrogenism combined with a history of irregular menstruation—usually very infrequent—fulfills the diagnostic criteria for what is called classic PCOS, and this is the subset of women with PCOS who are at high risk for metabolic issues.
“I call this ‘internist PCOS,’” said Dr. Dunaif. “In contrast, women who are concerned about the cosmetic effects of androgens, like excess hair growth and acne, but are ovulatory do not appear to be at significant risk for associated metabolic problems.”
Dr. Dokras added that “taking the time to explain how the diagnosis is made based on the Rotterdam criteria and what phenotype the patient fits into” can help patients understand long-term comorbidities.
Some patients may think that a PCOS diagnosis means they won't be able to get pregnant or that it will be extremely difficult to do so. On that front, “I feel like the prognosis is a lot better than people often think,” said Heather G. Huddleston, MD, a reproductive endocrinologist and director of the PCOS clinic at University of California San Francisco Health. “For most of our patients with PCOS, we're able to help them without a lot of intervention in many cases.”
It is critically important for patients with PCOS to understand that the related reproductive abnormalities are ameliorated with age and that many women can conceive without fertility treatments in their mid-30s, Dr. Dunaif continued. Women with PCOS also reach menopause later, which prolongs their reproductive lifespan. “I tell my patients that this is the silver lining of having PCOS,” said Dr. Dunaif. Recent studies have confirmed that women with PCOS do not have fewer children than unaffected women, she said.
A patient-centered approach
PCOS is a chronic, lifelong, heterogeneous group of disorders, which can make it challenging to treat and study.
“It's not a gynecologic disorder alone,” Dr. Dokras said. “It's an endocrine disorder which has gynecologic manifestations, dermatologic symptoms, and cardiometabolic comorbidities, which is where the [primary care physicians] can play a very important role. These patients have a high prevalence of depression and anxiety, which is also an opportunity for primary care physicians to intervene.”
Once a diagnosis is established, “the most important role of an internist is to try to make sure that complications down the street are prevented and mitigated,” said Dr. Shekhar. In patients with PCOS, physicians should screen for associated conditions like obesity, cardiovascular disease, sleep apnea, and metabolic dysfunction-associated steatotic liver disease (formerly nonalcoholic fatty liver disease), among others. In addition, “there's a very well-documented increased risk for type 2 diabetes, about a fourfold increased risk” in these patients, said Dr. Dunaif.
PCOS can make it difficult for patients to manage their weight and is linked with a heightened risk of anxiety, depression, body image distress, and disordered eating, Dr. Dokras said. One study published by Annals of Internal Medicine in February found that patients diagnosed with PCOS in Taiwan had an 8.47-fold increase in risk for a suicide attempt, although Dr. Dokras noted that no other studies have found a similar association. Additional research published in Neurology, also in February, revealed an association between PCOS and lower cognitive performance and lower white matter integrity in middle-aged women.
Patients have a significantly higher prevalence of obstructive sleep apnea (OSA), and, for the first time, the 2023 guidelines include a recommendation to screen for its symptoms. PCOS is also linked with a heightened risk of endometrial cancer and anovulatory infertility.
But not every patient is going to have all of these complications, Dr. Dokras stressed. When it comes to treatment, “there's no one answer to, ‘How are you managing PCOS?’ It depends on the presentation of the patient, what is bothering the patient the most. It needs to be patient-centric, and so it's not just a one size will fit at all.”
To manage PCOS, physicians first have to ask themselves what symptoms the patient is reporting and what's most relevant, she continued. “Then we systematically approach their symptoms.”
If a patient's primary issue is menstrual irregularities, birth control pills are typically prescribed. However, for patients who can't be on birth control—say due to clotting issues—then metformin can be used.
“About 50% of women who take metformin will get regular periods back, and they'll often be ovulatory,” Dr. Dunaif explained. Metformin has the added benefit of potentially improving weight and lipid profiles, but it does little to treat hyperandrogenism. And although it will make women ovulate, those interested in fertility will do better on either clomiphene citrate or off-label letrozole, she said.
Patients with irregular menses and male hormone issues could go on oral birth control pills or a progesterone IUD. With adequate contraception, they can also be prescribed the antiandrogen spironolactone off-label at a dose of up to 200 mg daily, which has potential teratogenic effects on a male fetus, Dr. Dunaif continued.
However, patients looking to get pregnant and seeking treatment for excess male hormone symptoms typically won't be able to address them, “because either the treatments are birth control pills … or they're agents that block male hormones that can cross the placenta and interfere with the masculinization of a male fetus,” Dr. Dunaif explained. “So we don't want women to get pregnant when we're treating their male hormone excess.”
Many patients with PCOS present with overweight or obesity, but women who are relatively lean can also have the condition, explained Dr. Shekhar. Often, these women “are not appropriately screened, or the diagnostic threshold tends to be erroneously higher in the minds of physicians,” he said.
Regardless of weight or body mass index (BMI), lifestyle management, including healthy eating and exercise, benefits most patients with PCOS and is often recommended as first-line treatment.
“Obesity is such a significant driver of this syndrome, and even modest weight loss will help resume regularity in the menses and will bring down the androgen levels,” said Dr. Dokras. “Lifestyle management also improves depression symptoms” and can improve quality of life and decrease anxiety.
However, for some patients struggling with weight, lifestyle management may not be sufficient. Weight loss can be hard to maintain, and patients may regain the weight. Because of this, medical management should be offered early on, instead of making these patients feel guilty, Dr. Dunaif said.
The 2023 guidelines support use of antiobesity medications like liraglutide, semaglutide, and glucagon-like peptide-1 (GLP-1) receptor agonists to manage higher weight in PCOS patients.
Small, investigator-led studies have shown that GLP-1 receptor agonists are effective for weight management in PCOS, Dr. Dunaif said, but the medications aren't indicated for PCOS, in part because manufacturers are hesitant to support trials in reproductive-age women due to concerns over exposure in pregnancy, she said.
A 2019 review published by Reproductive Biomedicine Online found that GLP-1s were more effective than metformin in improving insulin sensitivity and reducing BMI in PCOS, but researchers concluded the available evidence was “inconclusive given its moderate to low quality.”
PCOS in primary care
According to experts, primary care physicians have the skill set, expertise, and opportunity to improve outcomes for patients.
“Because it has ‘ovary’ in the name, [PCOS] has been relegated to being a reproductive disorder and just never made it to mainstream internal medicine, and that's a tragedy,” Dr. Dunaif explained. “Although reproductive issues are important in young women, it's really the associated metabolic issues [with PCOS] that have major health consequences.”
Dr. Dokras described primary care physicians as being on the front lines of weight management: “Counseling the patient about that long-term management is really critical. The role that the primary care physicians and internal medicine physicians can play is in counseling patients about lifestyle management and screening for cardiometabolic risk,” she said.
Internal medicine physicians can also improve diagnostic delays, which may be due to the fact that “some physicians aren't as comfortable with what the criteria are or how to pull that information together and make a judgment call,” said Dr. Huddleston. Even though the condition is common, “I think the number of doctors out there that really feel comfortable making the diagnosis maybe isn't enough.”
She suggests physicians familiarize themselves with the diagnostic criteria and basic treatment strategies. “Most of [the strategies] are things that I think primary care doctors often do perform for other patients. It's just a matter of being comfortable that this is a treatment that we would use for PCOS,” Dr. Huddleston said.
One relatively simple way to improve diagnosis rates is to incorporate basic screening questions into check-ups.
“The best thing to do would be for all physicians who deliver primary care to learn to take a menstrual history, which isn't hard,” said Dr. Dunaif. PCOS patients can have very few menses per year, usually from the time when they started menstruating. “It's not a subtle symptom, just health care providers don't ask about it,” she said.
In addition to a menstrual history, physicians can ask patients if they have excess hair growth in areas they would not expect and if that's problematic, said Dr. Shekhar.
The diagnostic delays patients experience “really add a lot, both in terms of the health care cost and comorbidity burden, because these women are not promptly diagnosed. They're not promptly screened for other abnormalities,” he said.
Screening more women and having a low threshold of detection will cut down both diagnosis times and health care spending, Dr. Shekhar stressed. If “we pick up these cases early, we screen them appropriately, and then we manage the underlying disorder as well as the comorbidities well, I think we can make a huge impact in the lives of these patients,” he said.