MKSAP Quiz: Foot pain following catheterization
A 68-year-old man was admitted to the hospital 3 days ago for a non-ST-elevation myocardial infarction and underwent cardiac catheterization via the right groin. Today, the patient reports pain in his left toes and diffuse soreness in the left calf. Medical history is significant for hyperlipidemia and hypertension. Medications are aspirin, atorvastatin, metoprolol and lisinopril.
On physical examination, temperature is 37.8°C (100.1°F), blood pressure is 132/82 mm Hg, pulse rate is 68/min, and respiration rate is 14/min. BMI is 22. Dorsalis pedis and posterior tibial pulses in both feet are normal; femoral and popliteal pulses are intact. No femoral bruit is present.
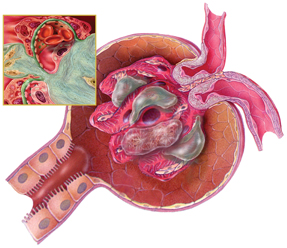
A photograph of the left foot is shown.

At admission, serum creatinine level was 1.2 mg/dL (106 µmol/L); it is now 2.2 mg/dL (194 µmol/L). Leukocyte count was 5000/µL (5.0 × 109/L) and is now 9000/µL (9.0 × 109/L) with 6% eosinophils. Erythrocyte sedimentation rate is 63 mm/h. Hansel stain of urine sediment demonstrates eosinophils.
Which of the following is the most likely diagnosis?
A. Acute interstitial nephritis
B. Cholesterol embolization syndrome
C. Contrast-induced nephropathy
D. Delayed hypersensitivity reaction
Answer and critique
The correct answer is B: Cholesterol embolization syndrome. This question can be found in MKSAP 16 in the Cardiology section, item 53.
The patient most likely has cholesterol embolization syndrome. This syndrome may present as a systemic illness, with fever, elevated leukocyte count and erythrocyte sedimentation rate, and with constitutional symptoms of fatigue and generalized muscle soreness. Patients may develop a red-purple to blue discoloration of the toes (seen in image) along with livedo reticularis, a lace-like purplish discoloration of the skin (not well visualized in the image). This patient has atherosclerotic disease documented by cardiac catheterization. Following cardiac catheterization, the patient developed pain and discoloration in the left toes, acute kidney injury, low-grade fever, elevated erythrocyte sedimentation rate, and leukocytosis with marked eosinophilia. These features are consistent with the cholesterol embolization syndrome.
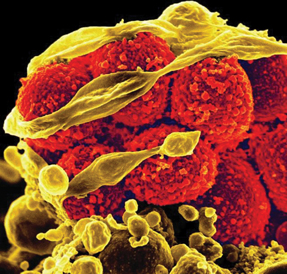
Embolization of cholesterol crystals may occur spontaneously in patients with severe atherosclerotic disease or following endovascular manipulation. Embolization involves small arterioles and capillary beds, and large vessel pulses are generally not impaired by the process. Toe involvement may progress to necrosis and eschar with tissue loss. Acute kidney failure may occur with significant embolization to the kidneys.
Treatment of the cholesterol embolization syndrome is primarily supportive. Anecdotal reports have suggested a possible role for LDL apheresis, iloprost, or corticosteroids. These therapies have not been evaluated in humans in a randomized fashion or in an animal model, however, and cannot be advocated for generalized use.
Acute interstitial nephritis can result in acute kidney injury and eosinophiluria, which is best detected by Hansel stain. Acute interstitial nephritis is usually caused by a hypersensitivity reaction to a medication, most commonly ß-lactam antibiotics and proton pump inhibitors; certain infections; and autoimmune conditions. Contrast-induced nephropathy is not associated with a systemic reaction such as that seen in this patient or with a painful discoloration of the toes. Similarly, a delayed hypersensitivity reaction would not cause a localized distal digital reaction.
Key Point
- Signs of cholesterol embolization syndrome include a red-purple to blue discoloration of toes, livedo reticularis, and signs of systemic illness, including elevated leukocyte count and erythrocyte sedimentation rate.