MKSAP Quiz: Evaluation for increasing fatigue and dyspnea with exertion
A 41-year-old man is evaluated in the emergency department for increasing fatigue and dyspnea with exertion. He was recently diagnosed with acute uncomplicated cystitis and started a course of nitrofurantoin 3 days ago.
On physical examination, temperature is normal, blood pressure is 106/72 mm Hg, pulse rate is 104/min, and respiration rate is 16/min. Oxygen saturation is 98% breathing ambient air. He has conjunctival icterus. Other than tachycardia, the physical examination is normal.
Laboratory studies:
- Haptoglobin: Undetectable
- Hemoglobin: 8.8 g/dL (88 g/L)
- Leukocyte count: 10,000/μL (10 × 109/L)
- Platelet count: 200,000/μL (200 × 109/L)
- Reticulocyte count: 18% of erythrocytes
- Lactate dehydrogenase: 458 U/L
Direct antiglobulin test is negative for IgG and C3. Peripheral blood smear shows microspherocytes, bite cells, and blister cells.
Nitrofurantoin is discontinued.
Which of the following is the most appropriate additional management?
A. Erythrocyte transfusion
B. Plasma exchange
C. Prednisone
D. Rituximab
E. Symptom monitoring
Answer and critique
This content is available to MKSAP 19 subscribers as Question 73 in the Hematology section.
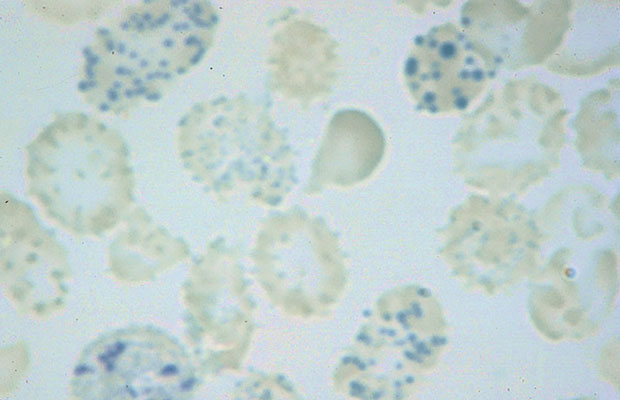
Clinical observation and symptom monitoring are appropriate for this patient (Option E). He is experiencing an acute hemolytic event related to glucose-6-phosphate dehydrogenase (G6PD) deficiency that was likely triggered by recent medication exposure. G6PD deficiency is an X-linked disorder and the most common enzyme deficiency affecting erythrocytes. It provides a survival advantage against Plasmodium falciparum and is, therefore, more common in persons of African, Asian, Mediterranean, and Middle Eastern descent. Enzyme deficiency results in failure to generate nicotinamide adenine dinucleotide phosphate (NADPH), leading to reduced glutathione levels and subsequent hemolysis, which is both intra- and extravascular. Acute hemolytic events can be triggered by oxidative stress, with medications and infections among the most common causes. Nitrofurantoin is one of the medications known to cause significant hemolysis in G6PD deficiency. Patients have signs of hemolysis on laboratory testing, and microspherocytes, bite cells, and blister cells are seen on the peripheral blood smear. Special stains can demonstrate denatured globin chains attached to the erythrocyte membrane (“Heinz bodies”) as shown. Semiquantitative tests are used to evaluate enzyme function through reducing NADP to NADPH. However, G6PD levels may appear normal during acute hemolytic episodes when brisk reticulocytosis occurs because reticulocytes have higher G6PD activity than older erythrocytes.
Managing hemolysis in a patient with G6PD deficiency includes removing the offending agent and providing supportive interventions such as packed red blood cell transfusions if needed (Option A). Patients typically recover within several days of drug discontinuation. This patient is no longer taking nitrofurantoin, and his hemoglobin level does not necessitate transfusion, so further intervention is not necessary.
No evidence of microangiopathic hemolytic anemia is seen in this patient's examination, with no reported schistocytes and a normal platelet count; therefore, a diagnosis of thrombotic thrombocytopenic purpura is not plausible, and plasma exchange would not be necessary (Option B).
This patient shows no evidence of an autoimmune process, including a negative direct antiglobulin test; therefore, neither glucocorticoids nor rituximab is indicated (Options C, D).
Key Points
- In patients with glucose-6-phosphate dehydrogenase deficiency, acute hemolytic events can be triggered by oxidative stress, with medications and infections among the most common causes.
- Patients with glucose-6-phosphate dehydrogenase deficiency have signs of hemolysis on laboratory testing, and microspherocytes, bite cells, and blister cells are seen on the peripheral blood smear.




