Patients and priorities in prostate cancer care
Prostate cancer requires men to work through a multitude of treatment options, and if the patient ends up settling on active surveillance, then the internist's role is even more important moving forward.
As prostate cancer patients cope with treatment decisions, and various side effects that might result from the path they select, primary care physicians can help quarterback their care through these phases and often many years of survivorship.
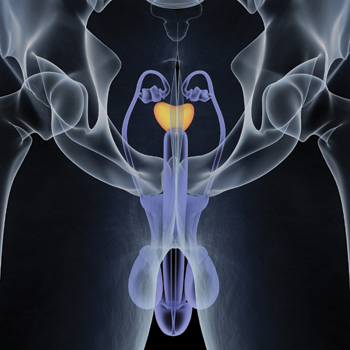
Nearly 161,000 U.S. men are diagnosed annually with prostate cancer, and roughly 6 million are living today with the disease, according to data from the National Cancer Institute. The malignancy, while potentially serious and life threatening, requires men to sort through a mix of options, some of which may not be effective or necessary and can cause side effects that persist for months to years after treatment has been completed.
“This is chronic disease management,” said Timothy Wilt, MD, MPH, MACP, a professor of medicine at the Minneapolis Veterans Affairs Health Care System. “And the internist needs to be actively involved and knowledgeable about the natural history of prostate cancer and the benefits and harms of treatment options, rather than abdicating their health care role to the specialists.”
Moreover, if the patient ends up settling on active surveillance, Dr. Wilt said, than the internist's role is even important moving forward. “They are really placing the trust in you that this is the right approach for them,” he said.
Dr. Wilt helped to author one of several long-term studies published recently, part of an expanding body of research showing no significant mortality difference for men with localized prostate cancer, regardless of whether they choose observation or treatment.
His study, published July 13 by the New England Journal of Medicine (NEJM), followed up on the outcomes for 731 men initially randomized to radical prostatectomy or observation from 1994 through 2002. After a median of 12.7 years, there wasn't a statistically significant difference in overall mortality or prostate cancer mortality between the two groups.
Another NEJM analysis, published Oct. 13, 2016, followed 1,643 British men randomized to one of three options—prostatectomy, radiotherapy, or active surveillance—and also didn't find any mortality difference. After a median follow-up of 10 years, the prostate cancer survival rate was at least 98.8% in all three groups; some of the men on surveillance had gotten treatment in the intervening years.
Increasingly, men with low-risk prostate cancer are opting for surveillance, according to data from a national registry of 45 U.S. urology practices published by JAMA in 2015, looking at trends from 1990 to 2013. From 1990 through 2009, no more than 14.3% of men selected surveillance as their initial approach. From 2010 to 2013, 40.4% did.
Still, even when doctors take the time to explain surveillance along with treatment options, it's always against the backdrop of the “cancer” word, said Ian Thompson Jr., MD, vice president of oncology for CHRISTUS Santa Rosa Health System in South Texas and a long-time prostate cancer researcher, who has promoted surveillance as a viable option.
Dr. Thompson has had patients walk out of his office comfortable with surveillance until they relay their decision to loved ones. “And they say, ‘He has cancer and his doctor is not doing anything about it.’”
Supportive decision-making
In this context, when the patient is meeting with various oncologists, the primary care doctor can provide a vital additional perspective, said David Penson, MD, MPH, professor and chair of the department of urological surgery at Vanderbilt University Medical Center in Nashville, Tenn.
“The primary care doctor is going to be viewed as, and hopefully is, an unbiased participant,” Dr. Penson said. “They should be relatively agnostic.”
Ideally, the primary care doctor already has some insight into patients' priorities, along with their general medical condition and the malignancy's aggressiveness, Dr. Penson said. Perhaps a man is nearing his final years of life, or is beset by other medical issues, so a typically slow-growing malignancy is not as much of a concern. Perhaps he admits that his sexual years are behind him. Or perhaps he's terrified of impotence and the other potential side effects of treatment.
Quality-of-life findings from the British study published last year in NEJM involving 1,643 men with a median age of 62, part of a study dubbed ProtecT (Prostate Testing for Cancer and Treatment), showed that effects from surgery and radiotherapy might linger for years.
At the start of the study, 67% reported erections firm enough for intercourse versus, after six months, 52% in the surveillance group, 22% in the radiotherapy group, and 12% in the prostatectomy group, according to the findings.
Urinary incontinence data showed that 1% of men among all three groups reported, at the study's start, using an absorbent pad. Among the surgery patients, that likelihood was 46% after six months and 17% by year six. The incontinence rate among radiotherapy patients was 4% by the sixth year and 8% in the surveillance group.
While some single-center studies report side effect numbers that don't run as high as population studies, Dr. Penson suggests that primary care doctors rely on the population data when they discuss potential side effects with patients, unless they can access data from the center where they're referring the patient. If population data are relied upon, search for subsets that might reflect the patient who is sitting in the office, for example, someone who is under age 65 in robust sexual health, he said.
Doctors also can reassure their patients that if they opt for active surveillance, they will be closely monitored for any worrisome symptoms or test results and the primary care doctor will coordinate with the cancer physicians, Dr. Penson said.
“I think it's important to frame active surveillance as an equivalent treatment in low-risk patients to surgery or radiation,” said Dr. Penson, noting that in the past it was almost offered up as an afterthought. “Doctors by their nature are risk adverse. They don't want to take any chances because they've been entrusted with someone else's health,” he said. “And patients hear the word ‘cancer’ and their head explodes.”
Side effect management
Sometimes patients are so grateful after surgery that they don't share or much dwell upon erection or other difficulties, Dr. Penson said. “They don't want their surgeon to feel like he or she didn't do a good job.” The patient's primary care doctor is more likely to hear about such frustrations in the weeks or months to follow, he said.
Rashid Alsabeh, MD, FACP, an internist and senior staff physician at Detroit's Henry Ford Health System, agreed. Often, the patient is more preoccupied in the first year or two with the prostate-specific antigen (PSA) readings and making sure the cancer is gone, he said.
“After that, when they are not that worried about the cancer any more, then they start to ask, ‘OK, is there anything else we can do to help with the erectile dysfunction? Is there anything else we can do to help with the urinary incontinence?’”
Primary care doctors are already familiar with the various erectile dysfunction medications like sildenafil (Viagra) and tadalafil (Cialis), among others, Dr. Alsabeh said. Patients who don't report benefit can be referred to their urologist to discuss other options, such as penile injections. But in his experience, patients are more frustrated over the long haul by incontinence—leakage severe enough to require regularly wearing a pad—than erection difficulties.
Following surgery, the most likely cause of incontinence is stress-related, Dr. Thompson said, in which the urinary sphincter is not strong enough to prevent leakage. In that case, medications are not likely to be helpful, he said. Instead, he suggested that the primary care doctor refer the patient to a clinician, most likely a urologist or a physical therapist, who can teach pelvic floor exercises.
When the leakage frustrations follow radiotherapy, it's more likely to be prostate obstruction, which treatment can exacerbate, Dr. Thompson said. The man's symptoms might be eased by one of several medications on the market for overactive bladder, such as oxybutynin (Urotrol) or solifenacin (Vesicare).
If the patient has persistent and lifestyle-limiting incontinence, such as soaking pads multiple times a day or wetting the bed at night, Dr. Thompson suggests a referral to a specialist to discuss the possibility of an artificial sphincter. “I have seen men who after having it placed reflected that a) their life had been transformed and b) that they wished they had done it earlier,” he said.
Lingering effects?
Regardless of the treatment approach, the primary care doctor should coordinate with the oncologist on PSA testing to clarify who is doing it, how often, and how the results will be interpreted, particularly if the man has chosen surveillance, Dr. Penson said. He noted that “the PSA can bounce around a bit” and said it's important that the nuances of the results are understood and explained to the patient.
Among men who get radiotherapy, there is a slightly elevated risk of bladder and colorectal cancer, and thus any potential symptoms should be evaluated, according to a 2015 review of the American Cancer Society's prostate cancer survivorship guidelines by the American Society of Clinical Oncology. Some that might develop, sometimes as long as four to five years after radiotherapy has ended, include blood in the urine, burning during urination, or painful or bloody bowel movements, said Dr. Penson, an author on the 2015 review.
“I think it's much more likely to be a side effect of the radiation [than cancer],” Dr. Penson said. But since patients likely aren't seeing their radiation oncologists at that point, their primary care physician should ask about and pursue any symptoms with colonoscopy or other testing, he said.
Men who are prescribed androgen deprivation therapy must be advised that side effects might include not only hot flashes, decreased energy, and other menopausal symptoms but also a heightened vulnerability to osteoporosis, Dr. Penson said. But, he added, there's an ongoing debate regarding how frequently these men should be screened, as well as when and whether bisphosphonates or other bone medications should be prescribed.
“They don't necessarily need to be treated,” Dr. Penson said, “unless they start to show signs of osteoporosis. There is an area of debate in this space as to how aggressive you need to be.”
A recent review and meta-analysis, published Sept. 5 by Annals of Internal Medicine, looked at the use of bisphosphonates and denosumab in men with nonmetastatic prostate cancer on androgen deprivation therapy. Researchers found that the medications did improve bone mineral density, a surrogate marker for fracture risk, but none of the studies were sufficiently powered to determine whether they reduced fractures. Denosumab was similarly found to improve bone density; one study did identify a reduction in radiographic spinal fractures.
While the systematic review was well done, Dr. Wilt said, he noted a number of limitations to the meta-analysis, including that the studies involved were mostly small and short-term and that the data on clinically evident fractures were limited.
Improving bone density “may mean that it will eventually prevent fractures that patients can notice,” said Dr. Wilt, but he remains doubtful. “It likely will mean treating many patients for a long time, and that means many patients are treated unnecessarily.”
But Dr. Alsabeh believes that it makes sense for primary care doctors to monitor a prostate cancer patient's bone density, along with other potential physical and mental effects, including state of mind in patients who have opted for surveillance. Neither the recently published British study nor Dr. Wilt's analysis found any significant difference in mental health symptoms between the treatment and nontreatment groups.
A patient's personality frequently guides their initial decision, Dr. Alsabeh said. “People who tend to be really anxious and really nervous, they tend to choose treatment,” he said. “That's probably better for them, so they don't keep worrying every day and every symptom they have.”
Occasionally, however, a patient on active surveillance will start “to really be overworrying” about the risk of the cancer spreading, Dr. Alsabeh said. Or a patient's mindset might shift after a loved one succumbs to the disease. In that event, Dr. Alsabeh said, he'll refer patients back to an oncologist to reconsider treatment options.



