DynaMed Plus Quiz: Shortness of breath
A 40-year-old trophy-winning professional knitter reports increasing shortness of breath and dry cough for the past week, as well as hoarseness and throat pain for the past three days. She has a 30 pack-year smoking history but had no respiratory symptoms before this week. Upon questioning, she reports feeling “feverish” and being unusually tired of late. She has no significant medical history, family and social history are noncontributory, and she is on no medication.
On review of systems she reports stiffness and pain in multiple joints in her hands and both wrists over the past two months, which she attributes to intense preparation for an upcoming knitting tournament. The stiffness is worse with inactivity, and the pain has not responded to acetaminophen. For the past few days she has been too weak to practice her knitting, and due to inactivity her hand symptoms have worsened, along with her respiratory symptoms.
On physical examination, the patient appears tired and has an occasional nonproductive cough. Her vital signs are normal other than mild tachypnea and an oral temperature of 100.2°F. Both hands are slightly enlarged and warm; she keeps them in her lap in open flexion and resists moving them. There is no overt deformity, but her wrists and the proximal interphalangeal joints of both index fingers are boggy and tender to palpation. Rales are auscultated in both lower lung fields. Her skin and ears, nose, and throat (ENT) are normal. She has no palpable lymph nodes, a nontender thyroid without palpable masses, a nontender abdomen without hepatosplenomegaly, and normal results on a neurological exam.
Laboratory test results include normal chemistries, a negative anti-nuclear antibody (ANA) test, and a normal complete blood count other than a leukocyte count of 13.8 × 109 cells/L with a small preponderance of neutrophils, a positive rheumatoid factor (RF), and a mildly elevated erythrocyte sedimentation rate. A chest radiograph shows moderate interstitial lung disease, and hand films are generally normal, without periarticular erosions of involved joints.
At this point, what is the most likely diagnosis?
A. Sarcoidosis and osteoarthritis
B. Rheumatoid arthritis (RA)
C. Systemic lupus erythematosus (SLE)
D. Community-acquired pneumonia with atypical bacteria
Correct answer: B. Rheumatoid arthritis (RA)
The combination of progressive joint and pulmonary symptoms worsening acutely over several days, together with a low-grade fever and lethargy, raises several diagnostic possibilities, including the four listed. The patient's joint symptoms are not very consistent with osteoarthritis but are most suggestive of RA: symmetric small-joint stiffness and acute clinical synovitis manifested by pain with any movement of the joint capsule. RA is one of the more common connective tissue disorders associated with interstitial lung disease, which matches the pulmonary symptoms, signs, and radiographic findings in this patient.
Lupus is also associated with nonerosive joint pain and interstitial lung disease, although pleural effusion is a more likely cause of rales in patients with SLE, and a negative ANA test is not common.
Sarcoidosis is the most common cause of interstitial lung disease; it can cause a false-positive RF and has multisystem manifestations, although joint involvement is not normally among them.
Community-acquired pneumonia by atypical organisms such as Mycoplasma pneumoniae is an important consideration as patients can present with fever, cough and arthralgia, but frank arthritis is rare, and the distribution and description of joint involvement are very suggestive of RA. This patient also had no laboratory evidence of hemolysis, although a cold agglutinin titer was not ordered. Also, acute cricoarytenoid joint inflammation, as seen in acute RA, might explain the patient's hoarseness and throat pain better than an infection, given the normal ENT examination.
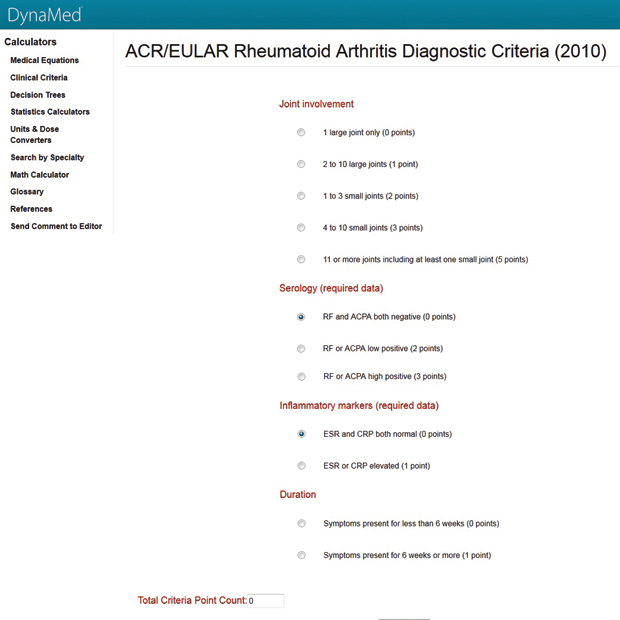
It is important to identify patients with RA as early as possible to begin therapy before irreversible erosive joint changes take place, which may begin as early as 12 weeks. The 2010 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) lists criteria for diagnosis of RA, published in September 2010 by Annals of Rheumatic Diseases. This patient has “at least 1 joint with definite clinical synovitis not explained by another disease,” but to be diagnosed with RA requires at least one other criterion, such as a score of at least 6 on the ACR/EULAR criteria assessing joint involvement, serologic and inflammatory markers, and duration of symptoms. Using a calculator such as the one in DynaMed Plus will quickly calculate a score of 7. This score justifies an urgent referral to a rheumatologist for assessment and treatment to increase the chance of a drug-free remission and reduce the risk for progressive joint damage.
The DynaMed Plus evidence summary for this question is online.