Can we stop the superbugs?
This issue covers antibiotic resistance among bacteria, ways to teach ambulatory care during a hospital residency, and a pair of stories about geriatrics.
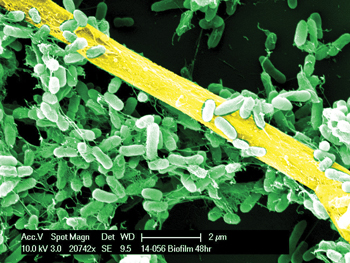
If you're in the mood for a good scare, our cover story this month may provide it. "Superbugs," or bacteria resistant to most or all available treatments, have been gaining a stronger foothold in the U.S. of late. In 2016, mcr-1, which confers resistance to colistin, was detected here for the first time, and earlier this year, a patient died of an infection that was resistant to all available U.S. antibiotics. In fact, resistance rates have been rising for many types of bacteria, and no end appears to be in sight. To fight these bugs, combating inappropriate prescribing and knowing the resistance and susceptibility patterns in your community are two crucial pieces of the puzzle. Staff writer Mollie Durkin offers more tips from experts on managing this growing problem, as well as a comprehensive overview of the biggest emerging threats on the infectious disease radar.
Another story looks at primary care, specifically the best ways to teach future primary care physicians when so much of residency is inpatient-based. Some programs have dedicated primary care tracks, while others offer seminars to help bring residents up to speed on aspects of running a practice, such as quality metrics and management of patient correspondence. Other programs, meanwhile, alternate training between outpatient and inpatient settings, focusing solely on one or the other at a time to avoid pulling residents' focus in different directions. Read our story to learn more about helping to foster primary care careers.
Also in this issue, two inside features look at geriatrics, specifically aging well. Our story discusses the best ways for physicians to help their elderly patients "age in place," that is, continue living independently rather than moving to nursing homes or other long-term care facilities. Physicians can start with a geriatric assessment, which one expert defined as covering four domains of functioning: physical, cognitive, psychological, and social. Eliciting patients' preferences and goals is crucial to determining next steps, while interventions such as a home evaluation to look for potential health hazards can help patients adapt to the restrictions of aging. A Q&A with geriatrician Thomas Perls, MD, MPH, FACP, the founding director of the New England Centenarian Study, offers an overview of the science of longevity and more advice on keeping elderly patients healthy.
This issue also includes the first column by ACP's new President, Jack Ende, MD, MACP. Read his thoughts on this page about the distinctions between evidence-based practice and evidence-based medicine, and why those differences matter.
How do you deal with antibiotic resistance in your community? What are your thoughts on training for primary care? Let us know.
Sincerely,
Jennifer Kearney-Strouse
Executive Editor