Guidelines get their own conference at G-I-N
A “high-stakes” effort is occurring in the pricey world of guideline development, as researchers around the globe seek to pool resources and find common ground.
A “high-stakes” effort is occurring in the pricey world of guideline development, as researchers around the globe seek to pool resources and find common ground to create and disseminate clinical recommendations.
“The practice of medicine needs to be aligned with evidence,” said Amir Qaseem, MD, PhD, MHA, FACP, Vice President of Clinical Policy at ACP. “But the average physician does not have time to read all the articles to simplify the research into recommendations. There are 15 million citations on MedlinePlus, with 10,000 to 20,000 added each week. Guidelines synthesize the evidence into actionable statements.”
Dr. Qaseem and hundreds of other physicians and academics evaluated guideline development and implementation, including clinical performance measures, at the 2016 G-I-N (Guidelines International Network) conference, held in Philadelphia in September with the theme “Individualized Guidelines and Clinical Performance Measurement in an Era of Personalized Medicine.” The meeting, which ACP co-hosted, was the largest G-I-N session ever held in the U.S., with 510 delegates from 33 countries involved in 5 plenary sessions, 30 workshops and panel sessions, and 70 oral presentations. Dr. Qaseem served as the conference co-president, while Annals of Internal Medicine Editor-in-Chief Christine Laine, MD, MPH, FACP, chaired the scientific committee.
“The whole purpose of the meeting is to bring the guideline and performance measures developers, implementers, policy people, providers, and payers together to discuss the implementation of evidence-based health care to improve health outcomes,” Dr. Qaseem said.
The role of performance measures is growing in the U.S. and globally, and most are based on clinical guidelines, Dr. Qaseem explained. Measures detect what level or quality of care physicians are providing, and they are being used to determine payment as well. This creates conflict for the physician, he said.
“Guidelines are based on data at population level, what is good for the majority of patients,” Dr. Qaseem said. “But ultimately you have to do what is best for the patient sitting in front of you. We can standardize certain elements of care but because there's a lot of variation from patient to patient, care cannot be converted into a factory assembly line.”
At the conference, one speaker presented a graph with data points that then turned into individuals' faces. “We need to keep individualized care in mind. We are treating patients; they are not data points,” said Dr. Qaseem.
Researchers at the conference also considered new ways to collaborate and combine resources. Just as research trials are registered, guideline development is registered so different groups know about each other's efforts.
Guidelines are high-stakes because they are so resource intensive, Dr. Qaseem said. Each guideline costs $300,000 to $500,000 to develop and takes about three years, and performance measures can add $200,000 and another two years to the process. “You're looking at half a million dollars in costs after five years, by which time the guideline is behind on the evidence already,” Dr. Qaseem said.
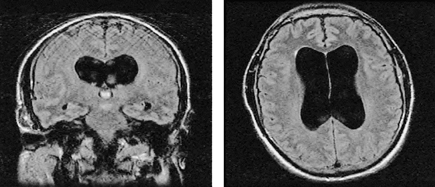
Also at the conference, delegates considered improving the model of guideline development that takes multiple chronic conditions into account. For example, the chance that a patient is being seen just for diabetes is low. Many people with diabetes also have hypertension or hypercholesterolemia.
“Having a guideline recommendation that addresses a single disease condition may not be enough for a physician,” Dr. Qaseem said. “What are you going to do with the more complicated patient, for example, one who is over 65 and is likely to have multiple chronic conditions? What should be the target levels for blood pressure or HbA1c in such a patient?”
Presenters at the G-I-N conference also tackled issues such as overdiagnosis, which Dr. Qaseem attributed to definitions of nonexistent diseases, such as the labels “prediabetes” and “prehypertension.”
“We tend to label people with a disease,” Dr. Qaseem said. “Patients get a diagnosis when it can bring more harm than good, including with unnecessary treatment.”