MKSAP Quiz: Impaired gait and balance
A 72-year-old man is evaluated for a 1-year history of progressively impaired gait and balance. He reports that he walks more slowly and is not as agile as he used to be, attributing a recently increased number of falls to not paying enough attention before tripping. In the past 6 months, he has had occasional problems recalling details of recent conversations and events, completing tasks around the house in a timely manner, and organizing and balancing his checkbook despite having been an accountant before retiring. The patient also reports some urinary urgency and frequency but otherwise feels well. He has hypertension treated with hydrochlorothiazide and no history of traumatic brain injury, meningitis, or intracranial hemorrhage.
On physical examination, vital signs are normal. General medical examination findings are unremarkable. On neurologic examination, gait is slow, with poor foot clearance, shuffling, multistep turns, and intermittent hesitation. Tandem gait is impaired. The remainder of the physical examination is unremarkable. He scores 23/30 on the Mini–Mental State Examination, with points deducted on the delayed recall and serial 7 calculation sections.
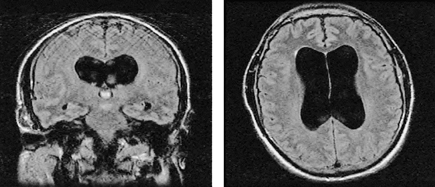
An MRI of the brain is shown.
Which of the following is the most appropriate next step in management?
A. Brain magnetic resonance angiography
B. Large-volume lumbar puncture
C. Trial of donepezil
D. Trial of levodopa
Answer and critique
The correct answer is B: Large-volume lumbar puncture. This question can be found in MKSAP 17 in the Nephrology section, item 20.
Large-volume lumbar puncture is indicated in this patient with likely normal pressure hydrocephalus (NPH). NPH is the most likely diagnosis in the setting of the triad of gait abnormalities, cognitive impairment, and urinary disturbance, especially when neuroimaging studies show enlarged ventricles out of proportion to cortical atrophy. NPH is a potentially reversible cause of cognitive and motor decline. A large-volume lumbar puncture with measurement of intracranial pressure and removal of 30 to 50 mL of cerebrospinal fluid (CSF) should be performed before consideration of placement of a ventriculoperitoneal shunt. Cognitive, balance, and gait examinations before and after the lumbar puncture can be useful to evaluate for potential response to shunting. If a positive response to the initial lumbar puncture is not seen and the clinical suspicion remains high, serial lumbar punctures or continuous lumbar drainage can be considered.
Periventricular white matter changes can be seen on the brain MRI and may have an identical appearance to what is seen in small-vessel vascular disease. However, without additional clinical or neuroradiologic evidence of a previous infarction, extensive evaluation with neurovascular imaging to assess for a cause of these radiologic changes on brain MRI is not warranted. Periventricular hyperintensities are a frequent finding in normal pressure hydrocephalus and are thought to be related to transependymal resorption of CSF.
The cholinesterase inhibitor donepezil is sometimes effective in improving cognitive symptoms and function in patients with Alzheimer disease but has no benefit for the gait and cognitive disturbances typical of normal pressure hydrocephalus.
Although this patient has evidence of lower-body parkinsonism, he lacks other findings that suggest the presence of idiopathic Parkinson disease, such as a resting tremor, asymmetric onset of motor symptoms, and typical nonmotor symptoms. Therefore, levodopa is not likely to result in any symptomatic benefit.
Key Point
- Large-volume lumbar puncture should be performed before placement of a ventriculoperitoneal shunt in patients with normal pressure hydrocephalus.




