MKSAP Quiz: Evaluation of chest pain
A 75-year-old woman is evaluated in the hospital 4 hours after onset of chest pain with findings of an ST-elevation myocardial infarction. She was taken emergently to the catheterization laboratory and underwent emergency percutaneous coronary intervention for a totally occluded vessel. Her post-intervention ventriculogram demonstrated a left ventricular ejection fraction of 30%. One hour after the procedure, she developed an acute arrhythmia. Medications are aspirin, metoprolol, atorvastatin, and clopidogrel.
On physical examination, the patient is afebrile, blood pressure is 100/60 mm Hg, pulse rate is 92/min, and respiration rate is 12/min. BMI is 25. Neck examination demonstrates cannon a waves. Cardiac examination demonstrates regular rhythm with a variable S1. Lungs are clear to auscultation.
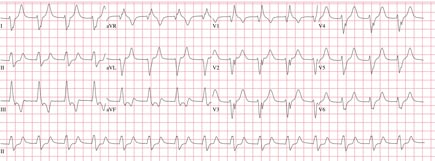
Electrocardiogram is shown.
Which of the following is the most appropriate management?
A. Amiodarone
B. Cardioversion
C. Implantable cardioverter-defibrillator
D. Lidocaine
E. No intervention
Answer and critique
The correct answer is E: No intervention. This question can be found in MKSAP 17 in the Cardiovascular Medicine section, item 42.
This patient requires no further intervention at this time. She developed a wide complex rhythm shortly after percutaneous coronary intervention and reperfusion of her infarct-related artery. The electrocardiogram (ECG) shows a regular wide complex rhythm at 92/min with no clearly discernible atrial activity, findings consistent with accelerated idioventricular rhythm (AIVR). AIVR is postulated to result from abnormal automaticity in the subendocardial Purkinje fibers. It is observed in up to 15% of patients who undergo reperfusion of an infarct-related artery. The rate is almost always less than 120/min and usually less than 100/min. Most studies have shown that it is a benign rhythm when it occurs within 24 hours of reperfusion. This patient is tolerating the rhythm well and is already on a ß-blocker for post–myocardial infarction care; therefore, no intervention is required.
Neither amiodarone nor lidocaine is indicated because AIVR is a benign ventricular arrhythmia and usually does not recur. Studies of prophylactic lidocaine after acute coronary syndromes have demonstrated potential harm, and amiodarone has been associated with decreased survival after myocardial infarction.
Cardioversion is not indicated because AIVR is a transient rhythm and, in this patient, it is well-tolerated.
AIVR usually indicates successful (or at least partial) reperfusion and is considered a reversible arrhythmia. Implantable cardioverter-defibrillator (ICD) placement is not indicated at this time given the patient's recent revascularization and nature of the arrhythmia. If the left ventricular ejection fraction remains low despite medical therapy, ICD placement might be indicated in the future.
Key Point
- Accelerated idioventricular rhythm is a common complication following coronary reperfusion and does not require intervention when it occurs within 24 hours of reperfusion.





