Improved BP control requires patients to change behavior
Physicians are working with patients on behavioral changes that might stave off the worst consequences of high blood pressure that occur later in life.
Hypertension has many physical effects on the human body, but the key to controlling it might involve a focus on behavior. Physicians are examining different ways to change patients' lifestyles through focused interventions that might ultimately prevent the consequences of high blood pressure.
Uncontrolled hypertension is one of the leading causes of premature death in the United States, accounting for an estimated 1 in 6 deaths in U.S. adults, according to a 2009 study that appeared in PLoS Medicine. In 2008, data from the National Health and Nutrition Examination Survey showed that only 41% of patients had their high blood pressure under control using either medication or other means. Exact estimates of patient adherence to blood pressure medications are difficult to pin down, but 1 study estimated that as many as 50% of patients prescribed antihypertensive medications stop taking the medication within 1 year.

“High blood pressure is a lifelong, progressive, and largely asymptomatic disease process,” said Matthew R. Weir, MD, FACP, professor and director of the division of nephrology at the University of Maryland School of Medicine in Baltimore. “Unfortunately, there is really no Pavlovian need for patients to continue to take their medications.”
As a result, patients may not always realize that uncontrolled hypertension can affect multiple organs and lead to significant morbidity. For example, a 2013 European study by Herttua and colleagues published in the European Heart Journal found that patients who were nonadherent to their blood pressure medications were almost 4 times as likely to die from a stroke and 3 times as likely to be hospitalized from a stroke than were adherent patients.
Reasons for nonadherence
The demands of taking medication for hypertension can create nonadherence, physicians agreed.
Polypharmacy is a well-recognized contributor. Many patients with uncontrolled blood pressure are asked to take more than 1 blood pressure medication, and many will also have related comorbidities such as high cholesterol or diabetes that also require medications.
“If you have diabetes, high blood pressure, high lipids, and heart failure, you may be taking as many as 14 prescription medications,” said Raymond R. Townsend, MD, director of the hypertension program at the Hospital of the University of Pennsylvania in Philadelphia. “The complexity of these regimens, with some medications that may have to be taken once a day and others 4 times a day, is a big hassle and difficult for many patients.”
Cost can also be an issue but is not usually as big a problem with hypertension as it can be with other conditions. Of the 5 to 7 available drug classes for hypertension, all have generic drugs available within them, making hypertension a fairly inexpensive condition to treat, according to Dr. Townsend. Education may more frequently be the problem, he added.
“Patients fail to understand how important these treatments are and stop taking them because they don't think they need them or they may make them feel bad,” Dr. Townsend said.
Patients may also stop taking blood pressure medication because of side effects, which are wide ranging and can include dry cough with angiotensin-converting enzyme inhibitors, peripheral edema with calcium-channel blockers, and sexual dysfunction with beta-blockers and diuretics.
“Some patients may not want to disappoint their physicians by discussing the difficulties they are having with their medications,” Dr. Weir said. “It is at least partly the job of the physician to query patients carefully to be sure that they are not having side effects.”
Interventions
Because the reasons behind nonadherence to hypertension medications can be multifactorial, lifestyle changes, including an improved diet and increased physical activity, are also important, said Sundar Natarajan, MD, an internist at the VA New York Harbor Healthcare System. Following the DASH diet, which is low in sodium and fat and rich in fruits and vegetables, equals 1 blood pressure lowering medication. If it is combined with regular exercise and weight loss, it could be as effective as taking 2 drugs. Increased monitoring can also help.
“Just scheduling regular visits to monitor blood pressure is the simplest form of an intervention to improve blood pressure and adherence that can be easily practiced,” Dr. Natarajan said.
One such intervention called “Check It, Change It,” headed by Duke University Medical Center in North Carolina, asked patients to regularly enter their self-monitored blood pressure data into an online program. Depending on patients' initial blood pressure levels, they also received ongoing behavioral and lifestyle counseling from a physician assistant, medication assessments, medication intensification as needed, and, for those with the highest blood pressure, at least 1 home visit to identify possible nonmedical barriers to control. At 6 months, the rate of blood pressure control among the study participants increased from 51% to 63%, according to results published last October by Circulation: Cardiovascular Quality and Outcomes.
Dr. Natarajan was an author of a similar study looking into a telephone-delivered tailored behavioral intervention designed to improve hypertension control among patients with repeated uncontrolled blood pressure.
Patients were assigned to a usual care group, where care was delivered as usual at an outpatient clinic and educational materials recommended by the American Heart Association and National Heart, Lung, and Blood Institute were provided; a health education intervention group that added monthly non-tailored telephone counseling for 6 months; or a tailored stage-matched intervention group that included a tailored monthly phone call with information on diet and exercise modifications and medications based on patients' readiness to change their behavior. After 6 months of the intervention, a greater percentage of patients assigned to the tailored intervention had control of their hypertension, according to results published in the February 2015 Hypertension.
Dr. Natarajan said the tailored intervention is different from many others because it applies the transtheoretical model or stages of change to diet, exercise, and medications, classifying patients with repeated uncontrolled hypertension as being in 1 of 5 stages for each behavior, with different counseling methods used for patients according to their stage of change:
- Patients in the precontemplation stage have no conscious intention to change;
- Patients in the contemplation stage plan to change but not within the next 6 months;
- Patients in the preparation stage are making steps to change and hope to take action within a month or are already changing their behavior;
- Patients in the action stage have made changes to their behavior but not for greater than 6 months; and
- Patients in the maintenance stage have changed their behavior and been maintaining those changes for longer than 6 months.
Dr. Natarajan said that clinicians can usually identify a patient's willingness to change by using only 2 to 3 brief questions. In their study, Dr. Natarajan and colleagues identified patients' readiness for change by first defining appropriate adherence to a behavior and then asking if patients were following that targeted behavior. If patients answered “yes,” the researchers asked how long they had been following that behavior. If they answered “no,” they were asked when they planned to do so.
To apply this type of program more widely, Dr. Natarajan recommended that practices initially identify only those patients with repeated uncontrolled hypertension, giving them a smaller number of patients to initially focus on.
At the University of Pennsylvania, Dr. Townsend said a new innovation center is focused on taking a multidisciplinary approach to blood pressure adherence and control.
“At the center we have social workers, pharmacists, nurses, and physicians who meet and discuss ideas for getting patients to get their blood pressure checked more often and to get them more on board with taking their medications,” Dr. Townsend said.
The program works best, he said, when the multidisciplinary team members brainstorm and use their own expertise or knowledge of each individual patient to come up with motivational methods that they think would work.
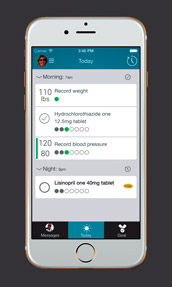
“One of the things we often approach patients about is investing in a blood pressure monitor, which helps patients buy into the illness and, consequently, behave a bit better,” Dr. Townsend said.
In fact, a 2013 study by Katrin Uhlig, MD, MS, and colleagues published in Annals of Internal Medicine found that patients who practice self-measured blood pressure monitoring, with or without additional support, were able to lower their blood pressure at 6 months.
More complex monitoring methods may be difficult for internists to implement, however, according to Dr. Townsend. “In the real world, internists often have 10 to 12 minutes with each patient to set the stage for their hypertension management,” he said.
In practices where behavioral interventions may not be realistic, physicians can take a few more immediate steps to try to improve blood pressure control.
Dr. Townsend recommended that physicians take a look at their own habits in an effort to combat physician inertia, such as failure to properly adjust a patient's hypertension medications when that patient is not meeting goals. Dr. Townsend mentioned a 2015 trial published in Blood Pressure that found that in multiple large clinical trials, as many as 15% to 37% of patients remained on the first dose titration step despite not having reached the target blood pressure goal. In order to combat this inertia, physicians must listen to each patient's feedback and work with him or her to find hypertension medications that best fit his or her needs, Dr. Townsend said.
Dr. Natarajan recommended that primary care physicians talk to nonadherent patients in private about the importance of their medication in a nonbiased manner. This method has been shown in research to improve adherence and provide a more lasting change in patients' behavior, Dr. Natarajan said.
“It is difficult for a patient to be honest about not following the medication treatment regimen, particularly where the medication is available at low or no cost,” Dr. Natarajan said. “It is important to ask questions in a non-judgmental and nonthreatening manner in order to get accurate, unbiased responses.”
Typically, before asking about adherence to treatment, a physician can frame the conversation as follows: “Many patients have difficulty taking pills as prescribed on a regular basis. Sometimes patients forget, miss their medications, or do not take it because they are feeling great or if the medicine causes them to feel worse.” Then the physician can ask about their adherence to medications. Dr. Natarajan said he also follows a similar format when asking about diet and physical activity.
Dr. Townsend echoed the importance of one-on-one conversations with patients about controlling hypertension.
“One big factor we found to be important in understanding patient medication-taking behavior is their perception of how much the provider cares about them,” Dr. Townsend said. “When they feel you have made eye contact, touched them in the course of clinical encounter, asked about something other than their salt consumption and exercise pattern, it seems to be important toward getting them to comply with their medical regimen.”