Searching for signs of eating disorders
Internists are often the first clinicians to see signs of an eating disorder, with the rapid or extreme changes in weight apparent both in person and from the history recorded in a patient's chart. But primary care clinicians may sometimes be afraid to ask about it because they are unsure how to handle what they might learn.
As the United States wages its war on obesity, roughly half of all adult Americans are on a diet on any given day. But between 20% and 25% of them will progress to partial or full eating disorders, according to the National Eating Disorders Association.
All told, nearly 24 million Americans are battling at least one of the three major eating disorders: anorexia nervosa, bulimia nervosa, and binge eating disorder. Ten million women and girls are afflicted with anorexia or bulimia, and although these disorders still predominantly affect women, 1 million men and boys grapple with them, as well.

Binge eating disorder, which will have its own category in the upcoming edition of the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM-5) to be published in May, is thought to affect 13 million Americans, 40% of them men.
Internists are often the first health professionals to see the signs of an eating disorder. A long-term patient-physician relationship will make rapid or extreme changes in weight apparent both in person and in a patient's chart.
But although they will be tasked with treating the medical complications of eating disorders, many internists don't screen for disordered eating, said Rosalind Kaplan, MD, FACP, medical director at Temple Health Women's Care and associate professor of medicine at Temple University School of Medicine in Philadelphia.
“Primary care physicians often won't ask because they're afraid of opening Pandora's box. They don't feel comfortable pursuing it within the time constraints of an office visit, and they're aware that treatment can be work-intensive if you're not familiar with it,” said Dr. Kaplan.
Even when internists do screen their patients, the secrecy and shame that go hand-in-hand with eating disorders make diagnosis a challenge, said Teri Pearlstein, MD, associate professor of psychiatry and human behavior and medicine at the Alpert Medical School of Brown University in Providence, R.I.
She said, “Your patients aren't going to come in and say, ‘I'm restricting or purging.’ They will often deny it because they're invested in the behaviors. Instead, they'll present with physical symptoms and signs.”
Diagnosis a moving target
The physical signs of disordered eating depend on the condition and its severity, but there is some overlap, particularly with anorexia and bulimia. According to ACP's Physicians' Information and Education Resource (PIER) module on eating disorders, which was co-authored by Dr. Pearlstein, patients with these disorders commonly complain of dizziness, headache, fatigue, heartburn, abdominal pain, bloating, constipation, amenorrhea or menstrual irregularity, loss of libido and cold intolerance.
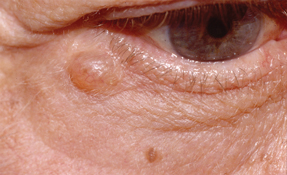
Upon examination, patients may be found to have bradycardia, hypotension, swollen parotid glands, pitting edema, brittle nails, muscle weakness or wasting, and dry, scaly skin.
Although a BMI lower than 18.5 kg/m2 should be a red flag for anorexia in the presence of these signs, patients with bulimia alone are often normal weight. Others may be overweight or obese, depending on whether their bulimia is coupled with binge eating.
“Just because someone is underweight or overweight, don't assume the person is not bingeing or restricting, respectively,” said Michael Rosen, MD, ACP Member, an internist and psychiatrist in private practice and a faculty member at Stony Brook University Medical Center in Stony Brook, N.Y.
Dr. Rosen added that eating disorders are often not static.
“Diagnostic criteria has been a moving target, and while binge eating is going to be incorporated [into DSM-5] as an individual diagnosis, I look at eating disorders as a spectrum disorder,” he said. “I can have a patient who is 80 pounds overweight with binge eating who a year later has developed anorexia and has a BMI of 17, and then the year after that will switch to bulimia and have a normal weight.”
The shifting nature of eating disorders makes a thorough, but skilled, history-taking paramount, he said.
“Here's where you put on your nurturing cap, and take an open, empathetic approach to the patient,” he said. “You're diving into something that has incredible shame wrapped around it, and you have to show that you care and you ‘get it.’”
Dr. Kaplan agreed. “I ask patients to tell me about their diet and exercise in a broader sense. Most will start to talk, and from there I can ask more pointed questions,” she said. Those questions will cover whether patients have concerns about their eating, and if so, what those are; whether they've been on a diet; or whether they have used purging techniques such as self-induced vomiting or laxative abuse.
The likelihood of straight answers depends on the eating disorder, she added. “Anorexics are more likely to fudge their answers. They're the most threatened when the illness is revealed. But many of my patients [with other eating disorders] have expressed relief that now it's out, because I'm acknowledging their disorder and normalizing it as part of a medical interview.”
Primary care physicians can zero in on potential eating disorders by using the SCOFF questionnaire, a series of five questions developed by British researchers in the late 1990s that have been adapted for use in the U.S. The PIER module adds several questions for further discussion. (See sidebar, “SCOFF Questionnaire and additional questions.”)
“What's nice about SCOFF is that it targets both anorexia and bulimia by focusing on loss of control and starvation. It's one of the better screens I recommend to primary care physicians and physicians in obstetrics and gynecology,” said Dr. Pearlstein.
Internists may encounter patients whom they suspect may have anorexia but whose cases are not clear. Testing the patient's leptin may help determine the diagnosis, said Deborah Mangham, MD, FACP, associate medical director at Park Nicollet's Melrose Institute, a Minneapolis facility dedicated to treating patients with eating disorders. “Leptin will be very low in a starving person, and normal in the constitutionally thin person,” she said.
Screening tools that may reveal binge eating disorder include the Bulimic Investigatory Test, Edinburgh (BITE) and the Binge Eating Scale (BES), both of which patients complete themselves. The BITE can be downloaded free as a Word document; the BES can be downloaded free from the National Cancer Institute's Grid-Enabled Measures Database.
Risk from every angle
According to the PIER module, groups at risk for developing eating disorders include adolescents with chronic diseases such as type 1 diabetes or gastrointestinal disorders; patients with a family history of eating disorders; overweight patients who have made multiple, unsuccessful attempts at weight loss or who have a history of weight cycling; and elite athletes.
Dr. Kaplan emphasized the importance of asking adolescents and college students about their participation in sports or other school programs. “Any activity where someone is judged individually and where weight or appearance are part of their performance can increase risk. For boys, they can include sports like wrestling, crew, or track. For girls it could be gymnastics or skating. But also consider activities like acting.”
Existing psychiatric conditions can increase risk, as well. People with depression, anxiety disorders and obsessive-compulsive disorder are more likely to develop an eating disorder, although there is often a question of which came first. Depression is a prime example of this, said Dr. Kaplan. “Is it primary depression with an eating disorder? Or is the depression because of the eating disorder?”
Assessing risk in patients with eating disorders is a double-edged sword for internists, who must be on the lookout for medical complications.
Patients who become malnourished as a result of anorexia or bulimia have increased risk of osteoporosis, cardiac arrhythmias, thyroid dysfunction, liver dysfunction, severe constipation, and loss of fertility. Those who abuse appetite suppressants may develop hypertension or anxiety, while those who abuse laxatives or diuretics may develop electrolyte abnormalities, abnormal gut motility, and secondary kidney failure. Patients who purge via self-induced vomiting may also develop dental cavities and worn tooth enamel.
For patients who gain extreme amounts of weight through binge eating, the risks of obesity apply, including metabolic syndrome and type 2 diabetes, cardiovascular disease, hypertension, dyslipidemia, gallbladder disease, joint and muscle pain, and diminished fertility.
Eating disorders may stand in the way of treatment for coexisting conditions, said Dr. Mangham.
“When patients purge, they may throw up medication,” she said. “Malnutrition makes antidepressants and other medications work less efficiently. People with type 1 diabetes might omit insulin to try to lose weight, and they will begin to get diabetes-related complications like retinopathy at a much younger age.”
Finally, when assessing risk, internists should consider that patients with eating disorders often have coexisting psychiatric conditions, said Dr. Rosen. “These patients usually carry more than one diagnosis,” he said. “If you suspect a patient of having an eating disorder, look for addictions. Not just drugs or alcohol, but also shoplifting, gambling, and sexual addictions. Patients with eating disorders are also more likely to have anxiety disorders.”
Studies indicate that 12% to 18% of patients with anorexia battle substance abuse, as do 9% to 55% of patients with bulimia. According to the Cleveland Clinic Center for Continuing Education, other comorbidities common to patients with eating disorders are depression (50% to 75%), sexual abuse (20% to 50%), obsessive-compulsive disorder (25% with anorexia nervosa), and bipolar disorder (4% to 13%).
Treatment
Experts agree that treating eating disorders can be a challenge from the get-go. Internists must address the need for treatment in a way patients will find acceptable, and if a patient is malnourished because of anorexia or bulimia, that can be an uphill battle, said Dr. Rosen. “Malnutrition changes the way the brain thinks, and the disorder begins to feed off itself. It takes over the individual, and causes the individual to do anything he or she can to prevent weight gain,” he said.
Dr. Mangham said that this distorted thinking is the primary source of denial in patients with eating disorders, especially those with anorexia. “Basically, anorexia becomes ego-syntonic, where it's acceptable. Patients don't want to change, are not willing to reveal their disorder, and have to be forced by family members to seek treatment.”
To try to help patients understand the importance of treatment, she suggests using concrete examples of what the disorder can do to the body.
“Almost all patients with anorexia or bulimia have bone loss,” Dr. Mangham said. “If you take a bone density test, you can show them that they have the bone density of someone decades older. It's not to scare them, but to make them more aware of the damage [the disorder] is causing.”
Dr. Mangham noted that patients with bulimia can be more amenable to treatment when the disorder hits a certain threshold. “Once it starts interfering with the person's ability to work, go to school, or participate in activities they enjoy, many of them do want to stop, especially if they also binge,” she said. “It's very disruptive to their lives, and that can motivate them to change.”
Overweight patients with binge eating disorder tend to be propelled toward treatment out of a desire to lose weight and to stop feeling remorse or guilt after eating, she added.
Once treatment is on the table, Dr. Rosen takes a four-pronged approach: medical stabilization, nutritional therapy, medication therapy and talk therapy. “The internist is crucial for the first step, because if the patient isn't medically stable, nothing else will work,” he said.
For patients who are malnourished because of anorexia or bulimia, stabilization may involve hospitalization or admission to a treatment facility depending on whether they are in imminent danger from organ damage. After that, the primary concern is weight regain, then psychotherapy or cognitive behavior therapy.
Research has not shown medication to be particularly effective for patients with anorexia. A literature review published online in Substance Abuse in March 2012 by researchers at the University of Florida noted that antidepressants were not effective in improving weight in anorexics, and that there is “limited evidence” that antidepressants improve anxiety and depression in this population.
The researchers noted that studies suggest the atypical antipsychotic olanzapine can increase body mass index for anorexics who binge and purge, but there is no evidence of this effect in those whose disorder is one primarily of restriction.
Other studies suggest that antidepressants, namely fluoxetine and sertraline, and the antiepileptic zonisamide can be effective in decreasing the “urge to purge” and the number of binge or purge episodes in patients with bulimia. The antiepileptic topiramate has been shown to have the same effects, but for patients who are overweight or obese because of binge eating disorder, there is the potential added benefit of weight loss.
Regardless, the threshold for referral to a mental health professional should be low, said Dr. Pearlstein. “Internists may wish to try these drugs for bulimia and binge eating disorder, but treating eating disorders will require the involvement of physicians, mental health professionals and nutritionists,” she said. “It's a team effort.”