When you look, but don't see the diagnosis
Gradual yet significant change in a woman's appearance, first noticed by a daughter she hadn't seen for a year, leads to the diagnosis of a common yet frequently missed ailment. Why hadn't those who'd seen the woman daily noticed anything? Intuitive vs. deliberative thought processes made all the difference.
Diana De Jesus, ACP Associate Member, a second-year internal medicine resident at Sound Shore Medical Center in New Rochelle, N.Y., told us about a 65-year-old woman who suffered from excessive sweating. The woman worked as a receptionist in a local nursing home. Her symptom had started five years earlier. At that time, she was evaluated by her primary care physician for profuse sweating, even in winter months, so severe that she often had to change her sheets at night. Her doctor attributed her symptom to menopause. Not long after, the patient reported large bunions and calluses on her feet that made it difficult for her to wear her shoes, and she was referred to a podiatrist. The patient was seen periodically by her internist and also by the podiatrist for the same complaints.
The patient had not seen her daughter, a college student living in the Midwest, for almost a year and traveled to visit her. When she arrived, her daughter exclaimed, “What happened to your face?” The daughter went on the Internet to see if she could figure out what might be responsible for the changes she noted in her mother's appearance. Quickly she happened on the diagnosis of acromegaly. Her daughter told her to go back and see her primary care doctor. The patient went to see him, asking, “Am I sick? My daughter thinks I might have a disease called acromegaly.” On specific questioning, the patient proved to have many classic symptoms of acromegaly, including increased snoring noticed by her boyfriend, increased ring size as well as shoe size, carpal tunnel syndrome, colon polyps and headaches.

The physician ordered an MRI scan, which showed a large pituitary tumor measuring 2.5 cm × 1.4 cm that was impinging on the optic chiasm. The patient was referred to an endocrinologist and laboratory testing confirmed the diagnosis of acromegaly: Her IGF-1 level was 897 ng/mL and her growth hormone was 73 ng/mL, both clearly elevated. The patient underwent transsphenoidal surgery, but the tumor could not be completely resected. She refused radiation therapy and was treated postoperatively with octreotide. With this treatment, growth hormone and IGF-1 levels returned to the normal range, and within weeks the patient's sweating subsided.
Dr. De Jesus saw the patient in the outpatient clinic as part of her endocrinology elective. “She had all the classic characteristics of acromegaly, coarse facial features, frontal bossing, spaces between her teeth, macroglossia, beefy hands with sausage-shaped fingers and very large feet with thickened heel pads. Doctors and nurses saw her every day at the nursing home where she worked,” Dr. De Jesus observed. “But no one noticed anything.”
Why was the diagnosis not made?
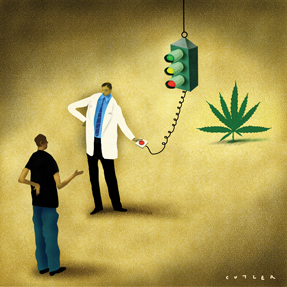
Acromegaly is a diagnosis that is often missed, even by experienced clinicians. We can gain some insight into why this occurs by looking at what cognitive scientists have categorized as the two systems of thinking: intuitive and deliberative. The diagnosis of acromegaly can be made intuitively, when the distinctive appearance immediately strikes a trained observer. There is virtually instantaneous integration of the signature findings, including characteristic facial features, large hands and feet, and sonorous voice, and this picture is then instantly associated with the diagnosis. This thought process occurs largely below the level of consciousness. An observer who sees a person on a regular basis is at a disadvantage in appreciating changes that occur over time due to what is termed the “contrast effect.” Studies of perception have shown that we notice differences more reliably when there is a significant contrast, in this case, a marked change from baseline appearance. The doctors and nurses who saw the patient every day could not appreciate the contrast in appearance because the changes occurred so gradually; they could not benefit from the contrast effect. But the patient's daughter, a college student without any medical background, was immediately struck by the contrast between the memory of her mother's appearance more than a year ago, and the woman she saw before her eyes.
As it happens, even a highly trained specialist can miss the diagnosis of acromegaly due to the contrast effect, as one of us, Dr. Hartzband, describes:
“Soon after completing my fellowship in endocrinology, I began to work with a senior endocrinologist who had been in practice for many years. One day, I saw a man in his late 60s with an acromegalic appearance sitting in the waiting room. I assumed he was here to see my colleague. ‘Is that your patient with acromegaly?’ I asked. ‘What patient with acromegaly?’ he responded. It turned out that this was the husband of one of his long-time patients with Graves' disease. His patient was Portuguese-speaking and her husband came to every appointment with her to serve as interpreter. The endocrinologist had seen this patient every six months for the past 10 years, but he did not make the diagnosis of acromegaly in her husband until it was pointed out, due to the contrast effect. This was the first time I had encountered this man, and fresh out of fellowship where I had just seen several cases of acromegaly, I was able to make the diagnosis. These recent cases from my training were prominent in my mind and readily recalled, what has been termed by cognitive scientists as an availability heuristic. Although availability can sometimes lead you astray, in this case it turned out to be helpful. Of course, when my senior associate had met this man initially 10 years ago, his appearance was not yet classic for acromegaly and the diagnosis was not at all obvious. And as he continued to see him regularly, he did not perceive the slow changes in the man's appearance.”
But all is not lost if the diagnosis is not made intuitively. We can use the second system of thinking that involves deliberation. The patient described by Dr. De Jesus did have symptoms that might have led to the correct diagnosis, including profuse sweating and enlarged feet. However, her primary care physician anchored on menopause as a cause for her sweating and bunions to account for her large feet.
It is valuable to use both kinds of thinking, intuitive and deliberative, in medicine. But this case of acromegaly points out potential pitfalls in both systems of cognition. Here, intuitive thinking was thwarted by a lack of contrast. Deliberative thinking was limited by anchoring. When a patient's symptoms persist, we should try to step back and look at the case with fresh eyes, generating as broad a differential diagnosis as we can, invoking the fundamental question, “What else could it be?”