Letters to the Editor
Readers respond about medical marijuana, mindful medicine, pharmaceutical reps, and more.
While medical marijuana is a welcome addition to the physician's armamentarium and it is encouraging that 14 states have legalized its use for medicinal purposes [“Marijuana requests: Relief or ‘permission’?”, ACP Internist, November/December 2010], unfortunately, it seems that many fail to consider the fundamental issue involved, i.e. a person's right to their own body. If that right is not recognized, no amount of evidence will sway those who believe they should legislate what others do with their lives or what physicians should be able to prescribe.
The Republican Party, at the behest of the Tea Party movement, has rightfully embraced the principles of economic freedom; would that they realize that the same arguments against government tyranny apply to government intrusions on the right to one's own body and realize restrictions on medicinal marijuana are part and parcel of socialized medicine.
Amesh A. Adalja, ACP Member
Butler, Pa.
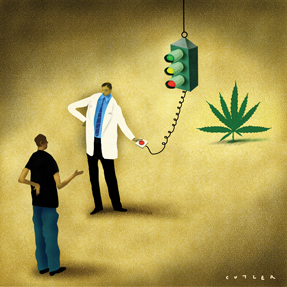
I was hopeful that the article on marijuana would inform internists about the lack of evidence to support its medicinal use. I was disappointed to find yet another article that doesn't provide any objective information about the evidence available in the literature regarding smoked marijuana for any medical indications. This is not what I would expect of my professional society. Dr. Kleber's assertion that there is not enough evidence for any physician to recommend marijuana to patients should have been the focus, not an afterthought near the end of the article. This issue deserves a thorough review of the literature and the potential risks of marijuana, not an opinion piece.
Kerstin Froyd, ACP Member
Denver, Colo.
Your article showed the obvious bias in the medical community against medical cannabis. As proven time and again, there are no median lethal dose issues, risks of liver damage or addictions and no logical reason that cannabis should be in a schedule 1 classification by our federal government.
Your use of the term “marijuana” rather than medical cannabis conjures back to the “Reefer Madness” era of the 1930s, and including what are easily refutable comments from the director of the Division of Substance Abuse at Columbia University confirms continued medical bias in favor of other, more harmful drugs and societal costs pushed by none other than “Big Pharma” in the eyes of the public.
With Arizona [Editor's note: After the story appeared, the state passed a medical marijuana ballot measure by 4,300 of 1.6 million votes cast], there are now 15 states that recognize the benefits of medical cannabis, and a vast majority of Americans are in favor of medical cannabis legislation, but as usual, the vested corporate interests, money trail and legal/corrections bureaucracy favor the status quo by continuing the failed “War on Drugs,” which has really been a “War on the 4th and 5th Amendments,” “War on (Some) Americans,” and “War on Plants,” for far too long! People in 15 states have spoken in favor of medical cannabis. ACP should listen to their patients rather than continuing to push other, much more harmful and expensive drugs when less risky alternatives exist.
Kevin J. Garcia
Albuquerque, N.M.
More on Mindful Medicine
The recent Mindful Medicine article that presented information about leprosy [“When patients don't tell all: The diagnostic challenge, “ ACP Internist, October 2010] was interesting and important given that leprosy continues to be imported and to occur domestically in the United States. However, the caption that accompanied the photograph of the nine-banded armadillo stated that “Americans who reside in the Southwest are at risk for leprosy due to contact with armadillos.” Americans who reside in areas where this armadillo has been found, especially in the Southeast and including Texas, are at possible risk for leprosy due to contact with armadillos. I have read that there is concern of it expanding its distribution north and west of this region. I have also read of patients with Hansen's disease in the Southeast United States who lacked foreign travel but did have armadillo exposure, and I have met a patient who stated they had eaten armadillo. It is also worth noting that leprosy is referred to as Hansen's disease in an effort to work towards its destigmatization.
Mark S. Dworkin, FACP, MPH
Chicago
Not for sale
I felt that I had to respond to the recent interview of Deborah R. Korenstein, ACP Member [“Guidelines getting tougher on industry, but physicians are not, “ ACP Internist, October 2010]. The tone of the article seems to be very negative regarding any interactions between physicians and pharmaceutical and/or device representatives. (I have not seen the publication in the Archives of Surgery.) Quite frankly, I am getting tired of the implication that my soul can be bought by a Chick-fil-A sandwich and a Dr Pepper.
Pharmaceutical representatives have a job to do, and that is to get doctors to write for their drugs. This type of marketing is done in almost every industry on Earth, and to think that medicine should be any different is ludicrous. They also bring much-needed samples to my office that I use to try patients on, at no cost to the patients, and that I use nearly every day to treat patients who cannot afford to purchase even generic drugs for their medical conditions. Some reps will even go out of their way to get me more medicine for these patients when I and they really need them.
I personally have no problem whatsoever with pharmaceutical lunches or small gifts that are medically related. I am personally insulted whenever I hear that my profession thinks that I am so weak that I can be swayed by a little food, a ballpoint pen, and some Post-it notes. Quite frankly, with reimbursements falling and expenses rising, I can use all the help I can get.
Do I think that pharmaceutical marketing has no influence on me? No, I'm not that naive. But it isn't as much of a problem as some academic do-gooders think it is. And I notice that there is no lack of pharmaceutical advertising in our medical journals.
Kyle G. Krohn, ACP Member
Lufkin, Texas
Corroborating perspective
In the Perspective article “Health care reform, PCMHs forge a new path for primary care “ in the October 2010 ACP Internist , there was a reference to a study of a five-person practice in terms of nonreimbursed work done. I did a study of my own practice over a six-month period, recording the same items but rather than reporting them in times per day, it was in times per every patient seen. It was published as a letter in Annals of Internal Medicine (2004;140:70) and it noted that I performed tasks outside of visits on 3.8 patients for every one patient seen in the office.
Because review of lab reports and consultation reports is considered to be reimbursed through the related visit, I also reported the numbers with those two activities removed, which was 2.45 per every patient seen. These numbers are likely similar to those reported in the Perspective article if a physician is seeing 20 to 25 patients daily, and further corroborates this degree of extra, unreimbursed activity by primary care physicians.
Robert A. Murden, FACP
Columbus, Ohio
Fed up with SGR
The letters to the editor in the November/December 2010 ACP Internist reflect the growing frustration among internists with the sustainable growth rate (SGR) stalemate. Today, finally, the issue made its way into the Denver Post's first section. Physicians are fed up with the annual battle to convince Congress to enact a temporary patch. This year we've been exhausted by no less than five such deadlines, wondering basically for the entire year how deeply we will have to dig into our business lines of credit to make payroll and pay the rent. And still, the best the American College of Physicians, the American Medical Association, the American Academy of Family Physicians and other groups can offer their constituencies is lobbying for yet another temporary “… reprieve that would give Congress time to work on a new payment system” Denver Post's words).
ACP leadership needs to wake up and realize how fed up we are with this stalemate, this Groundhog Day of a process. Lobbying has failed. Again, lobbying has failed. We are back at the same square one where we were a decade ago. It is time for the ACP, AMA, AAFP, and other groups to call for and lead a Medicare strike, whereby physicians refuse to see Medicare patients, except for urgent/emergent problems, for a period of, say, three days. By the way, don't call Grandma by phone and tell her that her appointment is cancelled. Let her struggle across town and up to the office with her walker, then tell her why she won't be seen that day, then hand her a piece of paper with the office phone numbers of her senators and representative on it. Maybe then we will see real change. If that doesn't work, strike for a week. Then two weeks. Then a month. It is obvious that only such action will get rid of the SGR.
Jay Kinsman, ACP Member
Colorado Springs, Colo.



