Filling in the GAPPs will strengthen evidence-based medicine
Little data supports the use of genomic testing for subjects such as warfarin dosing. Paradoxically, that lack of evidence leaves open the potential for the misuse of direct-to-consumer genomics tests for fun, or for their premature adoption by clinicians.
Clinical translational research seeks the answer to the fundamental question clinicians ask themselves daily: “If I use this (test, drug, device), will my patient's health improve?” Multiple evidence reviews for genomic applications have demonstrated that the answer is too often “There is insufficient evidence to recommend for or against use of X in the management of condition Y.” This unsatisfying conclusion repeatedly arises largely because of insufficient, or poorly executed, translational research.
The dearth of clinical translational research examining the clinical utility of genomic applications has far-reaching consequences, including fostering a reluctance on the part of busy clinicians to learn about genomics and a decreased willingness of insurers to pay for genomic applications. Often these barriers slow the incorporation of potentially beneficial new technologies into mainstream care.

Two recent evidence reviews illustrate this point: the CMS report on warfarin pharmacogenomics and a report from the NIH State of the Science Conference. They found extremely few studies have been conducted to support the use of warfarin pharmacogenomics to guide warfarin dosing or family history as a screening tool for risk of common disease in primary care, respectively.
Paradoxically, a lack of clinician knowledge and poor or absent reimbursement for genomic services can also result in premature adoption of genomic applications. This is most vividly exemplified by the controversial rise of direct-to-consumer marketing of genome-wide scans for health and recreational purposes.
Numerous influential groups have remarked on the lack of clinical translational research in genomics, including the President's Council of Advisors on Science and Technology and the Department of Health and Human Services Secretary's Advisory Committee on Genetics, Health, and Society (SACGHS). A 2009 SACGHS report noted, “In addition to the lack of underlying utility studies (and the lack of standards for judging those studies), there is no existing government or private-sector system capable of efficiently conducting utility assessments for the large number of emerging genetic tests.”
An attempt to develop a more coordinated national approach to translational research for genomics was launched. The new endeavor, supported in part by the CDC's Office of Public Health Genomics (OPHG) and the National Cancer Institute's Division of Cancer Control and Population Sciences, is known as the Genomics Applications in Practice and Prevention Network (GAPPNet). The organization, still in evolution, is shaping up to become a ground-breaking public-private partnership with a singular mission to integrate validated genomic knowledge into the practice of medicine, empower research and evaluation, and disseminate high-quality information on promising genomic applications in practice and prevention.
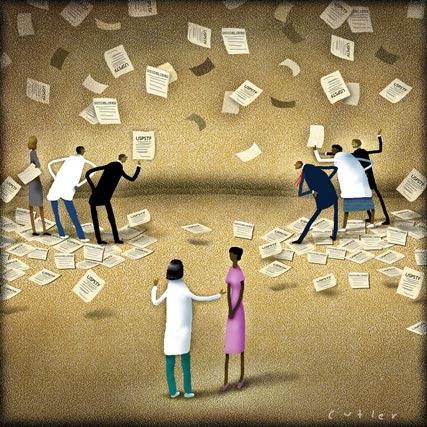
Groups represented at the meeting included a wide spectrum of perspectives from health care, including clinicians, insurers, industry, disease advocacy groups, academicians, and government groups from across the U.S. Despite the attendees' diverse and sometimes opposing viewpoints, there was a surprising and substantial agreement that the situation in the U.S. was unsustainable.
The metaphor brought up at the meeting was that the current status of genomics translational research resembled a boat with multiple oars in the water and no coordination of the oarsmen. The attendees agreed that a mechanism for national-level coordination of translational research, run by the groups that have a vested interest in effective and timely development of accurate and relevant data, would benefit all. GAPPNet would, in essence, be the coxswain.
GAPPNet will encompass four domains critical to the rational translation of genomic applications to health care. First, GAPPNet will facilitate rapid and transparent synthesis and dissemination of existing evidence regarding genomic applications. Second, GAPPNet will work to develop and disseminate evidence-based recommendations based on the best available information.
To achieve this, GAPPNet will build on the Evaluation of Genomic Applications in Practice and Prevention (EGAPP) program sponsored by OPHG. Groups like EGAPP and the U.S. Preventive Services Task Force are currently having difficulty keeping up with the rapid creation of new genomic applications for health care, leaving clinicians struggling for credible sources of information on the value of new technologies.
The third activity includes the coordination of existing translational research activities. At the federal level, this has already begun. The GAPPNet meeting provided a way to introduce funded researchers conducting translational research to one another in a noncompetitive, collaborative environment. Finally, GAPPNet will endeavor to find creative ways to create partnerships and sponsor additional translational research activities. This is a daunting task, given that high-quality translational research is costly and that public and private sectors face substantial financial constraints.
Some have argued that a more coordinated approach to the translation of genomic discoveries is unnecessary and destined to fail. This argument is based on the premise that the current slow diffusion of innovation in biomedicine serves as a Darwinian filtering process—only the most effective applications survive the test of time. Unfortunately, the status quo has contributed to the current health care crisis. New, costly, and not necessarily more effective technologies enter the system at a snail's pace and are even more slowly abandoned if proven to be less effective than cheaper alternatives.
Clinical applications arising from genomic discoveries are increasingly relevant to many aspects of health care delivery, and are coming at a soon to be exponential pace. Our patients, the field of genomics and our health care system can ill afford to ignore the opportunities that GAPPNet may provide to improve the translational research process over the upcoming decades.

W. Gregory Feero, MD, PhD, a family physician with a doctorate in human genetics, is Special Advisor to the Director of the National Human Genome Research Institute and a clinical associate professor at Dartmouth Medical School.