Letters to the Editor
ACP Hospitalist, ACP mobile content, ACP Press, and ACP QI programs.
Post-traumatic response
As a female veteran (‘06 RET), I am offended by the comment of Kurt Kroenke, MACP, that, “Because most veterans are still young men, I'd say if you have a young man come in with any unexplained physical and emotional complaints, a single question about whether he has been in a combat situation might be worth asking.” [“Post-war, vets face new battle with PTSD,” ACP Internist, September 2008.]
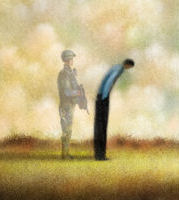
Female veterans are arguably subjected to more stresses than male veterans because they do not receive the hero's welcome accorded to male veterans. Their service to their country is not generally recognized and post deployment they are expected by our society to go straight back to their responsibilities to their family without any respite, in contrast to male veterans where there is no such expectation and, in fact, behavior bordering on dissolute is tolerated.
There are many older veterans, both male and female, from Vietnam whose issues have still not been addressed because the Vietnam veteran was marginalized by our society. Following Dr. Kroenke's advice would result in continuing to marginalize them and add in another forgotten group, the Iraq/Afghanistan female veteran who, in addition to the trauma incurred by men, also has a risk of being raped, a significant cause of PTSD.
Jean E. Howard, FACP
Address withheld by request
I read your article entitled “Post-war, vets face new battle with PTSD.” This is certainly an extremely important problem, and I believe that it is ruining the lives of many veterans who look as though they are perfectly okay and yet find themselves unable to function in society or support their families.
One aspect of the story that you didn't cover is that this might not be a psychological response to the dreadful experiences that the veteran might have had, but might be an actual physical injury. As you noted in your article, a high percentage of them have had a concussion with loss of consciousness. An even higher percentage have been exposed to blast, as from IEDs (improvised explosive devices). The risk for PTSD increases with the number of firefights. It is hypothesized that this reproduces a brain injury similar to that that occurs in decompression sickness, although the blast wave of increased followed by decreased pressure occurs much more rapidly than ascent from a dive. Interestingly, symptoms appear to get worse if the soldier is air evacuated. Divers who fly soon after a dive are risking decompression sickness.
If this mechanism plays a role, then hyperbaric oxygenation as used to treat decompression sickness might be effective. There are numerous case reports of improvements in traumatic brain injury of various types by this method, although at relatively lower pressures than are generally used for diving injuries. A formal study has been proposed, and funding is being sought by Dr. Paul Harch of New Orleans. In the meantime, some private facilities are undertaking to treat veterans.
While I am not myself providing this treatment, I am helping to support a veteran who is receiving it. After 20 sessions, the veteran says that he does not feel much different. However, he is no longer having daily migraines, which began after his injury. Moreover, he is driving a car which has been impossible for him, and reading a book. In the chamber he is observed to sit comfortably instead of constantly squirming. He would very much like to go back to work. He has not been able to go back to work owing to difficulties in concentration, flashbacks, and other seemingly psychological symptoms. The protocol calls for 40 treatments with a break after 20. So we'll see how he does.
Of course, no one is ever going to believe in the efficacy until a randomized study is done. Nevertheless, you might find it worthwhile to make physicians aware of this possibility. It may turn out to be the story of the decade!
Jane M. Orient, FACP
Tucson, Ariz.
Clubbing redefined
I read with interest the column “Mindful Medicine: Don't let emotion impede right diagnosis” [ACP Internist, September 2008]. I applaud the authors' tenacity with coming to two diagnoses that greatly assisted their patient. I am commenting because I believe a potentially inaccurate impression was left that digital clubbing is caused by hypoxemia. It also could be inferred that sleep apnea and/or carbon monoxide poisoning would be a likely primary cause of clubbing by leading to hypoxemia.
Clubbing is associated with processes that cause hypoxemia, as the authors state. However, it is a symptom of underlying processes through possibly neural mechanisms or presence of a circulating vasodilator that are typically inactivated as blood passes through the lung. This is the mechanism clubbing is thought associated with conditions such as congenital heart disease (shunt that bypasses the lung), bronchietasis (infection that causes AV-fistulas due to increased blood flow), and cancer (causing increased local blood flow, and shunt).
A quick reference can be found in at the eMedicine Web site, “Clubbing of the Nails,” by Robert A. Schwartz.
Holly Carveth, MD
Salt Lake City, Utah
Drs. Groopman and Hartzband respond: The applause should go to Dr. Moshe Chasky whose tenacity in pursing a diagnosis led to the improvement in the patient's condition. Our column was not meant to address the causes of clubbing, rather to emphasize that this physical finding led Dr. Chasky to search beyond the diagnosis of fibromyalgia. We thank Dr. Carveth for elaborating on the pathophysiology of clubbing with her letter and citation.
eRx redux
Thank you for the article on e-prescribing [“E-prescribing order hits unprepared internists,” ACP Internist, September 2008].
I have been using a stand-alone e-prescribing system (DrFirst) ever since Connecticut passed enabling legislation several years ago. Aside from safety issues, the chief benefit is in expediting the prescription renewal process. The old paper-based workflow for renewals involved a five-step process: receiving the request from the pharmacy or patient by phone or fax; retrieving the chart; managing the renewal; recording the event; and refiling the chart.
The new process, at its best involves only 3 steps: receiving the request from the pharmacy online, checking the patient's electronic chart (This is not always necessary.), and managing the renewal. The software keeps a record of the event.
Thus the new process saves time and labor by eliminating pulling the chart, refiling the chart and creating a paper record of the renewal. A convincing business case can thus be made for a positive return on invested capital based on this improved efficiency. However this only accrues when the system runs smoothly. Unfortunately the process does not always work this well, yet most barriers could be easily removed. Herein lies the opportunity for ACP to advocate for internists and their patients.
First, some pharmacies don't participate. Most chain pharmacies do but staff training and IT support is spotty. Many, but not all stand alone pharmacies are not participating. ACP should advocate for a federal mandate on pharmacies to enroll and use the SureScripts/RxHub exchange. After all, what is sauce for the goose is sauce for the gander, state's rights aside.
Second, mail order pharmacies never participate. ACP should advocate for mandatory participation by all mail order pharmacies. Using the postal system makes it a federal issue. Parenthetically, in my area Anthem (Wellpoint) has a pay for performance incentive that promotes e-prescribing yet the Wellpoint mail order pharmacy cannot or will not participate in e-prescribing!
Third, some prescriptions are for items covered under the Medicare Part B benefit. A good example is diabetic testing supplies. In order to bill Medicare the pharmacy needs testing frequency information and an ICD-9 diagnosis code. Pharmacies vary in their willingness to accept e-prescriptions even when those prescriptions contain this extra information. ACP should advocate for mandatory participation by all pharmacies and medical supply businesses that bill Medicare.
Fourth, the DEA has recently made e-prescribing of controlled substances more cumbersome and difficult. Lomotil (Schedule IV) prescriptions have to be printed, signed and faxed to the pharmacy or given to the patient. This is madness and ACP can help bring it to an end.
Rodney Hornbake, FACP
Essex, Conn.
Futile cases further considered
I agree with opinions expressed by Lachlan Forrow, FACP, in his column [Ethical Dilemmas, “Son's plea to prolong life at any cost sparks ethical quandary”, ACP Internist, September 2008.] I have been advocating for a strong statement/policy about futile treatments at our hospital for about 10 years. There has been agreement on the principle but a strong objection to developing a “Futility Policy”. More recently, there has been some acceptance to the idea of giving more authority to the doctors in the ICU. This, if accepted, would allow the ICU physicians to unilaterally withhold and override patient/family demand for CPR in patients with other advanced medical problems. The process has been initiated and hopefully will be complete in the next few months.
Despite the provisions of the New Mexico Healthcare Decisions Act, individual physicians, administrators and lawyers are reluctant and scared to override patient/surrogate demands even if they are for treatments that will not work.
Despite over 10 years of discussions, most physicians and institutions are not taking a stand. The Harvard system is unusual and has taken some bold stands. Hopefully, as more cases are ruled in favor of physicians and hospitals that refuse inappropriate treatments, the situation will improve.
Unfortunately, there is another movement from the ultra right wing, led by Wesley Smith that is taking the opposite stance. I am not sure what impact that will have on our practice.
Aroop Mangalik, MD
Albuquerque, N.M.
Abortion stance
Physicians should take keen interest regarding the role of abortion in the upcoming presidential election. Sen. Barack Obama's staunch support for the protection of women's rights and the abolition of religiously dictated dogma from laws is something he should wear as a badge of honor and physicians should applaud. For too long the Religious Right has dictated the terms of this debate with the emotional language that often makes no mention of the fact that this procedure involves a woman's body to which she has an inviolable right to do with what she chooses, as well as physician autonomy. As a pro-choice Republican I disagree with Sen. Obama on many issues, but it is on this issue that I will likely base my support.
Amesh Adalja, MD
Butler, Pa.



