MKSAP Quiz: Evaluation in the emergency department after chest discomfort
A 54-year-old woman is evaluated in the emergency department 3 hours after a 30-minute episode of chest discomfort. She is currently pain free. She reports a 2-day history of recurrent episodes of chest “fullness” while at rest. Episodes are 7/10 in severity and last 5 to 45 minutes without radiation or other associated symptoms. She also reports discomfort after meals. She has not exerted herself because of concerns of precipitating chest discomfort. She has no other medical problems and takes no medications.
Physical examination findings, including vital signs, are normal. BMI is 34.
Laboratory studies show a high-sensitivity troponin T level less than the 99th percentile upper reference limit; repeat measurement shows no change at 2 hours.
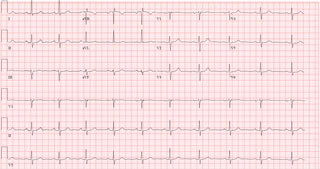
ECG is shown.
Which of the following is the most appropriate diagnostic test to perform next?
A. GRACE score
B. HEART score
C. Repeat ECG
D. Repeat high-sensitivity troponin T measurement
Critique
This content is available to ACP MKSAP subscribers in the Cardiovascular Medicine section.
The most appropriate diagnostic test to perform next in this patient with chest pain is the HEART (History, ECG, Age, Risk factors, Troponin) score (Option B). Initial evaluation of chest pain and possible acute coronary syndrome (ACS) includes an urgent ECG performed within 10 minutes of presentation, a thorough history and physical examination, and serial biomarker measurement. In the absence of significant ECG findings suggesting ST-elevation myocardial infarction, a summative risk score (e.g., HEART score) can help determine the likelihood of an acute ischemic process and establish the risk for 30-day major adverse cardiac events (MACE). When incorporated into a clinical decision pathway such as the HEART pathway, the score can identify patients at very low risk (~1%) who may be candidates for early discharge without additional immediate cardiovascular testing. This patient with a “slightly suspicious” history, normal ECG, age of 54 years, one risk factor (BMI >30), and a normal troponin T level has a HEART score of 2, suggesting a risk of 1% or less for MACE in the next 6 weeks. She can undergo further evaluation as an outpatient.
ACS risk scores such as TIMI (Thrombolysis in Myocardial Infarction) and GRACE (Global Registry of Acute Coronary Events) (Option A) provide prognostic information to guide treatment intensity in patients at intermediate or high risk for ACS but are less useful in identifying low-risk individuals such as this patient.
A repeat ECG (Option C), including one with alternate leads (posterior leads V7-V9), or serial ECGs may be considered in patients with a change in clinical status or if there is a high index of suspicion of evolving myocardial ischemia or injury. This patient has a normal initial ECG and no change in clinical status to suggest active myocardial ischemia. Further ECG studies are unlikely to provide useful information.
Repeat high-sensitivity troponin T measurements (Option D) have utility in identifying myocardial injury, especially in patients presenting very early after symptom onset or with clinical status change. Repeat testing in this patient with normal serial levels more than 3 hours after her last episode of chest discomfort is unlikely to provide useful information.
Key Point
- In patients presenting with chest pain, a summative risk score (e.g., HEART score) can help determine the likelihood of an acute ischemic process and establish the risk for a 30-day major adverse cardiac event.




