MKSAP Quiz: Slowly progressive dyspnea
A 30-year-old man is seen in the office for slowly progressive dyspnea that first appeared when walking rapidly or uphill. He denies orthopnea, palpitations, or chest pain. He has no other medical problems and takes no medications.
On physical examination, vital signs are normal. Jugular venous distention is present. There is a left parasternal impulse. A grade 2/6 systolic murmur is heard at the second left intercostal space, and a diastolic flow rumble is heard over the tricuspid valve. Fixed splitting of the S2 is present. The remainder of the examination is normal.
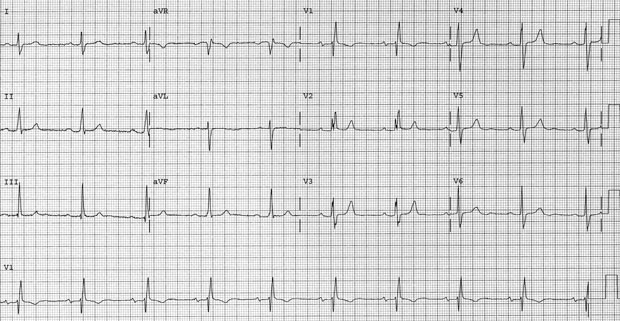
An ECG is shown. Chest radiograph reveals right heart enlargement, a prominent pulmonary artery, and increased pulmonary vascularity.
Which of the following is the most likely diagnosis?
A. Atrial septal defect
B. Bicuspid aortic valve with aortic regurgitation
C. Mitral stenosis
D. Ventricular septal defect
Answer and critique
The correct answer is A. Atrial septal defect. This content is available to MKSAP 19 subscribers as Question 113 in the Cardiovascular Medicine section.
An atrial septal defect (ASD) (Option A) is the most likely diagnosis in this patient. An ASD is a defect in the atrial septum resulting in a left-to-right shunt with eventual right-sided cardiac chamber dilatation in most patients. Adults with an ASD most often present with dyspnea, atrial arrhythmias, and/or right heart enlargement detected on cardiac imaging. Characteristic clinical findings include elevated central venous pressure, a right ventricular lift, and fixed splitting of the S2. A large left-to-right shunt causes a pulmonary midsystolic flow murmur and a tricuspid diastolic flow rumble owing to increased flow. This patient's ECG shows right axis deviation, incomplete right bundle branch block, and right ventricular hypertrophy, findings consistent with secundum ASD.
Aortic regurgitation due to a bicuspid aortic valve (Option B) causes a diastolic murmur at the left sternal border. The central venous pressure is generally normal, and a right ventricular impulse would not be expected. A systolic ejection click is often heard in patients with bicuspid aortic valve, but fixed splitting of the S2 is not heard. The ECG typically demonstrates a normal axis and features of left ventricular hypertrophy.
Patients with mitral stenosis (Option C) often present with dyspnea and atrial arrhythmias. The central venous pressure is often elevated, with associated pulmonary hypertension or tricuspid regurgitation. A right ventricular impulse may occur. An opening snap might be heard, followed by a diastolic murmur; this is generally best heard at the apex. Fixed splitting of the S2 is not heard. The ECG typically demonstrates left atrial enlargement.
Patients with a small (restrictive) ventricular septal defect (VSD) (Option D) are usually asymptomatic and demonstrate a loud holosystolic murmur along the left sternal border that often obliterates the S2. A thrill may be noted at the left sternal border. A right ventricular impulse would not be present. The ECG in patients with a small VSD is typically normal.
Key Points
- Characteristic clinical findings of an atrial septal defect include a parasternal impulse, fixed splitting of the S2, and a pulmonary outflow murmur.
- In patients with an ostium secundum atrial septal defect, the ECG demonstrates right axis deviation and incomplete right bundle branch block.



