The more you know … the more you know
Physicians should be in charge of health care teams because of the breadth and quality of their medical education.
Over the years, there have been many conversations, opinions, policies, and position papers addressing the issue of scope of practice in medicine. In 2013, ACP authored a policy paper to support team-based care led by physicians, due to their education, clinical training, and expertise. In addition, ACP has been a leader in promoting team-based care by creating a toolkit for its optimal implementation and management.
In personal conversations about scope of practice, I have had my own opinions, but I wanted to be more thought-provoking in my deliberations and discussions, acknowledging that physicians have at least 20 times as many supervised clinical hours as other health care clinicians, specifically nurse practitioners and physician assistants. I had to ask myself, is it just the quantity of clinical hours that makes us best qualified to lead our health care teams, or is there also something about the quality of those hours that supports physicians' value as team leaders?
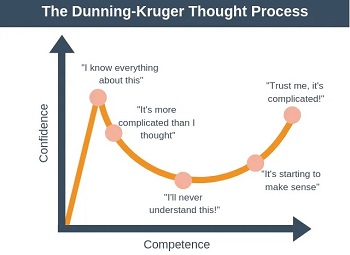
In my quest for an answer, I learned about the Dunning-Kruger effect, which was described by two psychologists, David Dunning and Justin Kruger, in 1999. The Dunning-Kruger effect is a theory of cognitive bias stating that people with more limited exposure to the depths of a task they are performing may not realize its breadth, making them both less able to consider all possibilities and less aware of the boundaries of their knowledge.
The Dunning-Kruger effect posits that the more exposure and years of experience a learner accrues, the more accurately they comprehend their true level of competence. Their confidence initially goes down, as they realize that the task is much harder than they originally understood. Through years of experience and encountering difficulties along their path, they gain a better understanding of the task's complexity, and their confidence and competence start to rise again, while still realizing the complexity of the task. The Dunning-Kruger effect supports the idea that some individuals with less in-depth knowledge are less able to make appropriate decisions in complex situations and that their knowledge gap prohibits them from realizing it.
To apply this theory to medical education, physicians are introduced to a wealth of knowledge in the preclinical years and throughout medical school. This process of information and work overload in itself minimizes overconfidence. As medical students transition to their clinical rotations, internship, and residency (cumulative clinical training hours), they are exposed to more than just the patient in front of them. In addition, they attend hospital rounds, morning reports, noon conferences, grand rounds, clinicopathologic conferences, and morbidity and mortality conferences, which provide a comprehensive exposure to the complexities of medicine.
As internal medicine physicians in training, we learn not only from the patients we care for but also from others on our team, through hospital rounds and education from attendings, through differential diagnoses in morning report to enhance our cognitive acumen and broad breadth of knowledge, through poor outcomes discussed during morbidity and mortality conferences to avoid future poor outcomes, and through the thoughtful approach of faculty systematically working through difficult medical cases in clinicopathologic conferences.
In internal medicine specifically, we have the opportunity to involve ourselves in the entire continuum of patient care, from the ambulatory setting, where we manage preventive care and chronic diseases, to the inpatient and ICU settings, where we manage more acutely ill patients. We quickly learn that the stable pneumonia patient seen in the ambulatory clinic can easily decompensate because we have also cared for a similar patient with pneumonia who presented to the hospital with respiratory failure, sepsis, and multiorgan failure. Thus, it's not just the number of hours learners are exposed to that impacts a physician's competence and confidence, but also the quality of those hours.
From the beginning of our medical learning and clinical exposure, we become aware of the difficulty and complexity of mastering the medical care of patients. Our initial training exposure, clinical experience, and multiple conferences that complement our learning keep us humbled in our confidence because we realize how much there is to know in medicine. However, over time, we continue learning, not only from our own experience and patients but also by absorbing learning opportunities, mistakes, and poor outcomes from our fellow colleagues with whom we train or practice.
When I compare the clinical exposure of physicians to that of other health care clinicians (who may desire independent practice), there is truly a large educational gap that goes beyond didactic education. Not only do other health care clinicians have fewer clinical hours and exposure, but the clinical hours they are exposed to have no set standards. While some programs may be well structured, others require each clinician to find their own source of preceptorships and clinical hours, with no regulation of quality or competence.
I believe the Dunning-Kruger effect applies to nonphysician clinicians because there is no consistent exposure to training to help them understand what they don't know. They are only exposed to what they see during their clinical experiences, which can easily create a sense of overconfidence. For example, a nonphysician clinician may work in a walk-in clinic and see a predominance of upper respiratory infections but not realize that one of those patients could be presenting with Wegener's granulomatosis or mucormycosis, since they have not been exposed to those learning possibilities. In the book “Patients at Risk,” the authors highlight the concept of the Dunning-Kruger effect, along with many other differences in the quality of training between physicians and other health care clinicians.
The intent of this column is not to belittle nonphysician clinicians, as there is an opportunity for all to have an integral role in team-based care, but rather to provide more insight and additional support regarding the unique qualifications of physicians' clinical training. Recent evidence also supports physician-led care: The Hattiesburg Clinic study, published in the Journal of the Mississippi State Medical Association in January 2022, demonstrated that physicians provide more high-quality and low-cost medical care with the highest patient satisfaction compared to other clinicians.
The value of physicians' medical clinical experience goes well beyond just the quantity of clinical hours. It's also the quality of those hours that amply justifies physicians' place as the leaders of their health care teams.




