MKSAP Quiz: Evaluation for chronic cough
A 42-year-old man is evaluated in the office for chronic cough. He first developed a cough 3 years ago. It is productive of clear to yellow sputum that is occasionally blood-tinged. He has taken antibiotics when his sputum production increases, after which his cough improves but never completely resolves. He has no dyspnea. He does not smoke cigarettes. He currently is taking no medications.

On physical examination, vital signs are normal. Oxygen saturation is 96% breathing ambient air. BMI is normal. Pulmonary examination reveals scattered inspiratory squeaks.
A chest radiograph shows ill-defined linear atelectasis and irregular peripheral opacities in the right and left lower lobes. A CT scan of the chest with contrast is shown below.
Which of the following is the most likely diagnosis?
A. Bronchiectasis
B. Centrilobular emphysema
C. Chronic bronchitis
D. Pulmonary Langerhans cell histiocytosis
Answer and critique
The correct answer is A. Bronchiectasis. This item is Question 81 in MKSAP 18's Pulmonary and Critical Care Medicine section.
The most likely diagnosis is bronchiectasis. Bronchiectasis is irreversible pathologic dilation of the bronchi or bronchioles resulting from an infectious process occurring in the context of airway obstruction, impaired drainage, or abnormality in antimicrobial defenses. The pattern of lung involvement varies greatly with the underlying cause and may be focal or diffuse. Bronchiectasis causes a chronic or recurrent cough typically characterized by voluminous sputum production with purulent exacerbations. The vast majority of chest radiographs are abnormal, typically showing linear atelectasis, dilated and thickened airways, and irregular peripheral opacities. High-resolution CT (HRCT) of the chest is the definitive diagnostic test for bronchiectasis.
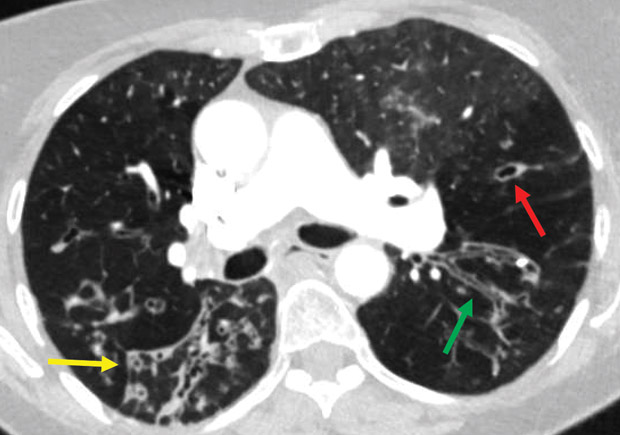
Typical findings (airway dilatation with lack of tapering [green arrow], bronchial wall thickening [yellow arrow], and cysts [red arrow]) may be seen on HRCT. In addition to imaging, the cause of the bronchiectasis should be determined. This may involve testing for chronic bacterial or mycobacterial infections, assessing for the presence of connective tissue disease, and evaluating immune function. In selected patients, testing for cystic fibrosis or α1-antitrypsin deficiency may be appropriate if suspected.
There is no evidence of emphysema on his chest CT imaging, which would typically appear as dilated airspaces, classified based on the distribution of abnormalities as centrilobular, panlobular, or paraseptal. Bullous or cystic changes may be seen.
Although the duration of his symptoms are consistent with chronic bronchitis, the chest CT scan shows evidence of bronchiectasis. In chronic bronchitis, the walls of the airways are thickened without dilation of the airways themselves.
Pulmonary Langerhans cell histiocytosis is a rare subacute interstitial lung disease of young, actively smoking adults. Patients may present with cough, fever, weight loss, and abnormal chest radiography. The chest CT findings include pulmonary nodules and cysts with midlung to upper-lung zone predominance and are not associated with bronchiectasis.
Key Point
- Chest CT is the definitive diagnostic study for bronchiectasis; typical findings are airway dilatation with lack of tapering, bronchial wall thickening, and cysts.




