Keeping up with cannabis
This issue also covers psoriatic arthritis, staffing for primary care, and social determinants of health.
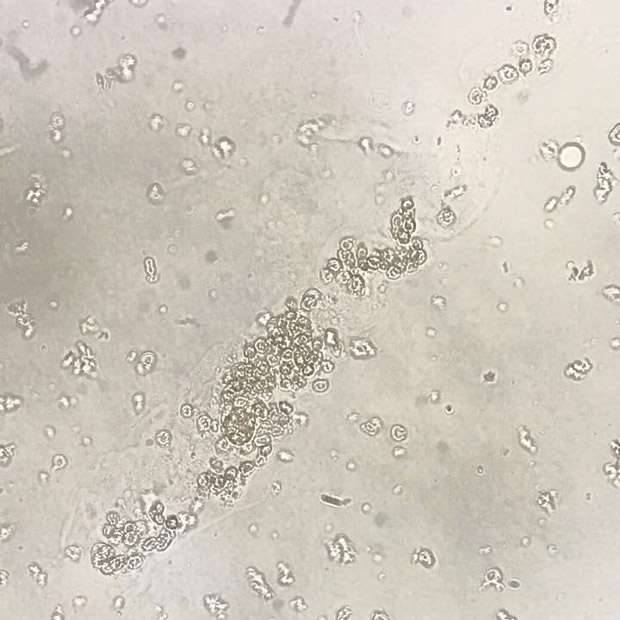
The changing landscape around cannabis use can be dizzying, for both patients and physicians. Medical marijuana is now legal in many states, and in the 10 states where recreational marijuana has so far been legalized, products containing the active ingredients in marijuana, tetrahydrocannabinol (THC) and cannabidiol (CBD), are also readily available. What's more, patients who are ingesting, smoking, or inhaling marijuana or related products may not be telling their physicians about them. But it's important to try to find out what patients are taking and to offer them guidance, since cannabis use can have negative effects. Staff writer Mollie Frost reviews the risks and benefits of the drug and how to address it, in all its forms, in clinical practice.
Speaking of changes, psoriatic arthritis has seen a fair amount of it lately, with a recent guideline detailing treatment options for a condition that once had very few. Internists are the first line of defense, especially since early diagnosis and treatment can ward off irreversible joint damage. Our story reviews the new recommendations about psoriatic arthritis and offers advice on what to look for during a physical exam, as well as tips on follow-up after subspecialist referral.
The ideal staffing for team-based primary care is a different puzzle for every practice. While the right mix of team members and job responsibilities can make a physician's job easier, gaps in expertise or vague or nonexistent job descriptions can make it much harder. Addressing staffing issues is never fun, but it's always worthwhile to figure out a practice's particular needs and make an effort to meet them, according to experts. Our story offers proven strategies and suggestions that can help physicians strike the right balance.
Patient partnership and the social determinants of health were the focus of two recent position papers from ACP, looking at working with patients and families as active partners in care and determining whether issues such as homelessness or food insecurity are affecting patients' health. An article offers advice on how internists can take these recommendations to heart in their practices and overcome challenges of implementation. And, Fatima Cody Stanford, MD, MPH, MPA, FACP, describes her experience on a 2018 flight and discusses what a doctor looks like.
This month, internists will gather in ACP's home city of Philadelphia for Internal Medicine Meeting 2019, networking with colleagues and friends and taking advantage of all the learning opportunities being offered. As always, our staff will be there too, bringing you the latest. Up-to-date news will be available via our Twitter feed and through our daily email dispatches. More meeting information, including registration, is online. If you're attending the meeting, let us know what you're most looking forward to by emailing us at immatters@acponline.org.
Sincerely,
Jennifer Kearney-Strouse
Executive Editor