New management for asthma flare-ups
Any patient with asthma may have a flare or asthma exacerbation, so primary care physicians should be aware of risk factors that might alert them to the patients who are particularly at risk.
Internists may want to consider modifying their approach to controlling asthma flare-ups after new evidence calls conventional management into question.
Recent data show that increasing inhaled corticosteroids (ICS) for patients with progressing asthma to prevent flare-ups, a widely conducted practice, has little effect. At the same time, asthma experts say new biologic therapies are generating promising results in the prevention and mitigation of exacerbations—if patients can afford the high price.
“This is so exciting because we're really getting beyond thinking about [asthma] as a stagnant disease,” said John Oppenheimer, MD, a professor at Rutgers New Jersey Medical School in Newark and associate editor of the Annals of Allergy, Asthma & Immunology. “We no longer think about asthma as one illness. It's a heterogeneous illness or, as some describe, a syndrome of multiple illnesses. What that means is no one therapy is going to result in resolution of this illness for everybody.”
Asthma flare-ups, characterized by worsened wheezing, shortness of breath, and/or coughing, are primary contributors to morbidity and mortality in asthma. The exacerbations are costly and often lead to lower quality of life, missed work, and increased acute visits to urgent care and hospitals, said William Busse, MD, an allergy and immunology specialist and professor at the University of Wisconsin School of Medicine and Public Health in Madison.
Patients with asthma exacerbations have markedly higher overall annual health care costs ($9,223 vs. $5,011) and higher asthma-specific costs ($1,740 vs. $847) compared with asthma patients without flare-ups, according to a 2012 study in the Journal of Allergy and Clinical Immunology. Patients who require acute care or hospitalization for asthma are at increased risk for future flare-ups and additional health care costs, the analysis found. Data suggest that asthma exacerbations may also result in progressive loss of lung function despite recovery from the acute event, said Dr. Busse, who coauthored an article about asthma exacerbations in the July/August 2017 Journal of Allergy and Clinical Immunology: In Practice.
“It is important for primary care physicians to realize that any patient with asthma may have a flare or asthma exacerbation,” Dr. Busse said. “Primary care physicians should also be aware of the risk factors … which will alert them to the patients who are particularly at risk for asthma exacerbations.”
Who's at risk?
Primary triggers for flare-ups include tobacco use, occupational exposures, and allergens, including those that are seasonal and perennial, said ACP Member Tatyana Gavrilova, MD, an assistant professor at Albert Einstein College of Medicine in the Bronx, N.Y., who specializes in adult and pediatric immunodeficiency and allergic disorders.
Tracking patient adherence with daily asthma medications is also important, since improper or inconsistent medication use is a top risk factor for exacerbations, Dr. Gavrilova said. Ensuring that patients recognize and communicate worsening symptoms to physicians in a timely manner is also essential. Patients who have a poor perception of symptom deterioration might benefit from the use of peak flow meters at home, Dr. Gavrilova noted.
“Knowing your patient well goes a long way,” she said. “Some people deteriorate within 24 hours; others take longer. You want to know how your patients' typical asthma flares progress and how early you need to intervene, how much and for how long.”
Adults with a history of previous exacerbations and severe disease—largely those patients requiring moderate to high ICS doses with or without other controller medications—are also predisposed to flare-ups, Dr. Busse said. Additional risk factors include the presence of eosinophilia, a history of asthma exacerbations, compromises in lung function, sinusitis and nasal polyps, and poor asthma control. Dr. Busse recommends that doctors make use of the Asthma Control Test, a website funded and developed by GSK, to determine a patient's level of asthma control.
“It is simple, consists of five questions, and requires less than five minutes to take,” he said. “The use of a questionnaire provides an objective measure of asthma control and also provides the patient with guidelines on what asthma control means and should be.”
Crafting an asthma action plan with patients can aid in the management of flare-ups as well. An asthma action plan includes information about exacerbation signs, direction about when to change or increase medications, and instructions on accessing medical care should symptoms progress. The Global Initiative for Asthma (GINA) 2018 pocket guide provides guidance on developing a plan.
“An asthma action plan is really a helpful tool to empower patients to intervene on their symptoms promptly,” Dr. Gavrilova said.
Research suggests protocol changes
Boosting ICS dosage at the first sign of worsening asthma symptoms has become routine practice, but recent trials suggest the regimen is not that effective.
An analysis of 1,871 adults and adolescents with at least one asthma exacerbation in the past 12 months found that quadrupling ICS dosage had only a modest effect of lessening flare-ups, according to the analysis, published in the March 8, 2018, New England Journal of Medicine (NEJM). A second study published in the same NEJM issue found that increasing ICS dosage fivefold in pediatric patients with worsening asthma symptoms made no significant difference in exacerbation rates versus children who continued current ICS doses.
The studies make a clear case for choosing an alternate strategy, said David J. Amrol, MD, an internist and allergist/clinical immunologist and associate professor at the University of South Carolina School of Medicine in Columbia, S.C., where he serves as allergy and clinical immunology division director.
“I no longer suggest quadrupling the dose of inhaled steroids for exacerbations because it was not effective in children and marginally effective in adults and actually carries the same systemic exposure as oral corticosteroids,” he said.* “[Instead], I provide patients with a five-day oral burst of oral steroids to use with exacerbations.”
Daily ICS are the preferred treatment for persistent asthma, but two recent studies suggest as-needed ICS with a long-acting beta-agonist (LABA) may be just as effective at reducing exacerbations. In the first study, investigators analyzed 4,176 patients ages 12 years and older who were given either twice-daily placebo plus budesonide-formoterol used as needed or budesonide maintenance therapy with twice-daily budesonide plus terbutaline used as needed. The analysis, published in the May 17, 2018, NEJM, and funded by AstraZeneca, found that while the as-needed regimen was not as successful at controlling day-to-day asthma symptoms, it was just as effective as the twice-daily regimen in preventing exacerbations.
The second study, published in the same NEJM issue and also funded by AstraZeneca, examined 3,836 patients ages 12 years and older who were randomly assigned to one of three regimens: twice-daily placebo plus terbutaline used as needed, twice-daily placebo plus budesonide-formoterol used as needed, or twice-daily budesonide plus terbutaline used as needed. Exacerbation rates with the two budesonide-containing regimens were similar, results found, although lower than the exacerbation rate with the terbutaline treatment.
The studies led Dr. Amrol to start using as-needed budesonide-formoterol in select patients with mild persistent asthma who do not want to take daily ICS and who are not bothered by mild increases in day-to-day symptoms. However, he noted that the indication is not FDA-approved.
“For patients that don't need daily therapy but are still at risk for exacerbations, this is a good option,” he said.
Stepping up treatment
Stepwise treatment to manage flare-ups depends on patient factors and asthma severity.
“Whether we're talking about stepping up or stepping down, our goal is to attain and maintain control,” Dr. Oppenheimer said. “Asthma comes in so many different shapes and sizes, our goal is really to optimize control, not just to attain control, but to maintain it through all of the triggers—colds, cold air, allergy, etc.—and then when we achieve that, to step down, if possible.”
GINA's updated 2018 global strategy for asthma management and prevention offers guidance about best practices when patients present to primary care or acute care settings with exacerbations. The guide recommends that physicians base their assessment of flare-up severity on the degree of dyspnea, respiratory rate, pulse rate, oxygen saturation, and lung function while starting short-acting beta-agonist (SABA) and oxygen therapy. From there, optimal treatment should include repeated SABA administration, early introduction of oral corticosteroids, and controlled flow oxygen, if available, according to GINA.
The update advises that ipratropium bromide be given for severe flare-ups and that clinicians consider IV magnesium sulfate for patients not responding to initial treatment. If signs of severe exacerbation are noted, or if patients act confused or drowsy or have a “silent chest,” primary care clinicians should make immediate arrangements for transfer to an acute care facility, the update advises.
Hospitalization decisions should be centered on several factors, including lung function, treatment response, history of exacerbations, and the patient's ability to manage treatment at home, the update said. Antibiotics are not recommended for exacerbations; because most flare-ups are caused by viral infections such as rhinovirus, antibiotics have limited benefit, according to experts.
Ongoing treatment strategies for patients with flare-ups should be based on the degree of worsening symptoms, according to the Asthma Yardstick, published in the February 2017 Annals of Allergy, Asthma & Immunology. For patients with mild persistent asthma that has progressed to moderate persistent asthma, for example, the Yardstick recommends three potential approaches:
- Use a low-dose combination of an ICS (e.g., beclomethasone dipropionate, budesonide, fluticasone propionate, fluticasone furoate, mometasone) with a LABA (e.g., formoterol, salmeterol, vilanterol);
- Increase ICS monotherapy from low dose to medium dose; or
- Add other medications (e.g., leukotriene receptor antagonist [LTRA], sustained-release theophylline) to low-dose ICS.
Regardless of the strategy chosen, the Yardstick suggests a three-month therapeutic trial with reassessment after six weeks. Recommendations for moderate to severe persistent asthma follow the same principles. For these patients, physicians can increase to a higher ICS/LABA dose and a higher-strength ICS and LABA combination as well as increase the dosage of ICS monotherapy or combination of ICS and LTRA, if necessary.
The blossoming of biologics
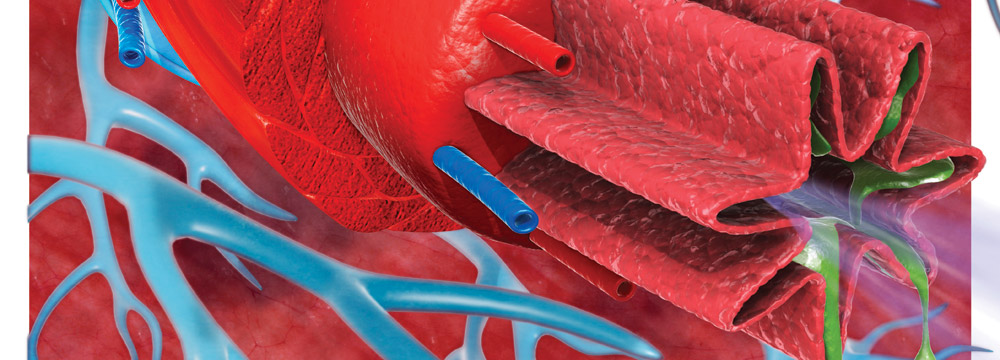
A burst of biologic therapies recently approved by the FDA offer new options for treating severe asthma. They target the asthma phenotype or specific characteristics of a patient's condition, such as increased mucus production or airway cellular and structural abnormalities, via the Th2 or T2 high phenotype (elevated eosinophils, exhaled nitric oxide and allergic subgroup), Dr. Oppenheimer said.
Omalizumab, for example, an IgG1k humanized monoclonal antibody, is recommended for patients with moderate to severe allergic asthma for whom other add-on therapies have failed, according to the 2017 Yardstick guidelines. Mepolizumab and reslizumab, two IL-5 antagonist monoclonal antibodies, have demonstrated efficacy in patients who have the eosinophilic asthma phenotype.
In the past year, additional biologic agents were approved for the treatment of severe, high-risk asthma, said Larry Borish, MD, FACP, a professor of medicine and microbiology at the University of Virginia in Charlottesville. These include benralizumab, which targets the IL-5 receptor, and dupilumab, which targets the IL-4 receptor. At least one newer agent, tezepelumab, which targets thymic stromal lymphopoietin, shows exciting promise in the treatment of this condition, he said. Dr. Oppenheimer added that this new agent is most exciting because it may provide efficacy in the T2 low subgroup, which he said thus far had no therapeutic option.
“Physicians need to understand the basis for the efficacy of these agents, exactly what they have been shown to achieve for asthmatics, and considerations regarding optimizing individualized therapies,” Dr. Borish said.
To this end, Dr. Borish and Dr. Oppenheimer authored a 2018 Asthma Yardstick update in the December 2018 Annals of Allergy, Asthma & Immunology that summarizes the latest approved biologics and details data on their effectiveness. One study, for instance, which was supported by Sanofi and Regeneron Pharmaceuticals and on which Dr. Busse was a coauthor, found that patients randomized to 200 mg of dupilumab every two weeks experienced a 47.7% lower rate of exacerbations annually than those assigned to placebo. The study appeared in the June 28, 2018, NEJM.
While data on the new drugs are encouraging, there remains a need for one-on-one studies to best assess which agent is most effective in which patient, Dr. Borish said. FDA approval and insurance guidelines regard eligible patients as those with severe asthma and evidence of an allergic inflammation, either IgE sensitization or an elevated eosinophil count.
“Thus [exists] a desperate need to develop a better basis for personalized medicine,” Dr. Borish said. “This is not something that pharmaceuticals will do, but as noted, there is currently a drive from the NIH to develop these studies. In the interim, for patients on maximum medical therapy who are still very poorly controlled or still high risk, strong consideration should be given to starting one of these agents.”
However, the high cost of the biologic agents also poses a barrier. The therapies cost between $28,000 and $30,000 per year, said ACP Member Jeffrey Tice, MD, a professor at the University of California, San Francisco, and lead author of a September 2018 Institute for Clinical and Economic Review (ICER) report that analyzed the cost value of omalizumab, mepolizumab, reslizumab, benralizumab, and dupilumab. The report concluded that none of the five therapies were cost-effective.
“The prices for all five of these biologics are really not in alignment with their clinical benefits,” Dr. Tice said. “Improvements in quality of life were relatively modest, [and] reductions in exacerbations were modest compared to placebo in the trials. Our estimates for all of these drugs were well above $300,000 for quality-adjusted life-year.”
In contrast, new therapies for hepatitis C are estimated at $20,000 per quality-adjusted life-year, according to Dr. Tice.
“Are [the asthma biologics] affordable for patients? Really, they're not,” he said. “When the list price is $30,000 a year, many patients have to pay some percentage of that list price. That's a big expense for patients.”
However, the therapies could ultimately save money if tailored to the correct patients with uncontrolled asthma, Dr. Oppenheimer said.
“It's very hard to reconcile their cost, but if we can be more precise and identify people [who] are high utilizers of the health care system [who have] a phenotype that would respond to these biologics, it could be life-changing,” he said. “And in theory, it could translate to more cost-effective medicine in the end.”



