MKSAP Quiz: Abrupt episode of syncope
A 40-year-old man is evaluated in the emergency department for syncope. He was attending a baseball game when he experienced a witnessed, abrupt episode of syncope while seated. He did not experience any prodromal symptoms. He sustained some facial trauma when he struck the railing in front of him. He has experienced near-syncope on several occasions in the past. His father died suddenly at age 50 years. The patient takes no medications and has no drug allergies.
On physical examination, the patient is afebrile, blood pressure is 125/64 mm Hg, pulse rate is 64/min, and respiration rate is 16/min. BMI is 26. Estimated central venous pressure is normal. Cardiac examination shows a regular rate with normal heart sounds and no murmurs. He has no peripheral edema.
Pertinent laboratory findings include a negative troponin test, a normal metabolic profile, and normal kidney function studies.
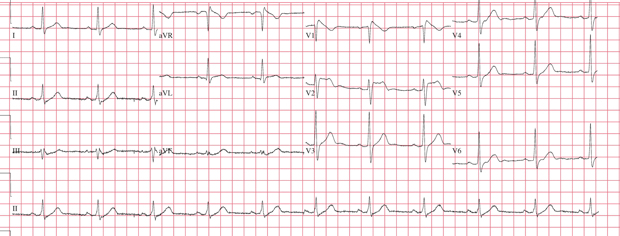
Electrocardiogram is shown. Echocardiogram demonstrates no structural heart disease and shows normal left ventricular function.
Which of the following is the most appropriate management?
A. Cardiac magnetic resonance (CMR) imaging
B. Exercise treadmill stress test
C. Implantable cardioverter-defibrillator placement
D. Tilt-table test
Answer and critique
The correct answer is C. Implantable cardioverter-defibrillator placement. This question can be found in MKSAP in the Cardiovascular Medicine section, item 68.
This patient should undergo placement of an implantable cardioverter-defibrillator (ICD). He had an episode of abrupt syncope that is concerning for a cardiac etiology, specifically an arrhythmia. He has a structurally normal heart on echocardiogram, but his electrocardiogram (ECG) shows right bundle branch block and 2-mm ST-segment elevation in the precordial leads. These findings are consistent with a type 1 Brugada pattern (coved or descendant ST-segment elevation followed by negative T waves) on ECG. The presence of a type 1 Brugada pattern and symptoms (cardiac syncope) or ventricular arrhythmia is diagnostic for Brugada syndrome. Brugada syndrome can be genetically heterogeneous, but it is often caused by mutations in the SCN5a sodium channel, which are believed to cause alterations in the ventricular refractory period and are responsible for the characteristic ECG findings and predisposition to sudden cardiac death.
Because this patient with Brugada syndrome is at risk for sudden cardiac death, particularly given his recurrent episodes of near-syncope and syncope, an ICD should be implanted. Patients with precordial ST-segment abnormalities should be referred to a cardiologist or electrophysiologist. Once Brugada syndrome is diagnosed, first-degree family members should be referred to an inherited arrhythmia clinic (electrophysiology clinic specializing in genetic disorders) for counseling and screening. Patients who have a Brugada pattern but are asymptomatic often do not require ICD placement. The incidence of Brugada syndrome is higher in patients of Asian ethnicity.
Cardiac magnetic resonance (CMR) imaging would not be helpful given the normal echocardiogram and diagnosis of Brugada syndrome. CMR imaging would be helpful if occult structural heart disease was suspected, such as cardiac sarcoid, amyloidosis, or arrhythmogenic right ventricular dysplasia.
An exercise treadmill stress test can be valuable for identifying an exercise-induced arrhythmia. Brugada syndrome often presents with nocturnal arrhythmias and is usually not adrenergically driven. A stress test would not aid in this patient's diagnosis.
Tilt-table testing should be reserved for patients with recurrent syncope without known heart disease or those with heart disease in whom a cardiac cause of the syncope has been excluded. Tilt-table testing may also be helpful in evaluating patients in whom documenting neurocardiogenic syncope is important (such as in high-risk occupational settings). In this patient, the ECG is diagnostic for Brugada syndrome and tilt-table testing is not needed.
Key Point
- The presence of 2-mm or more coved precordial ST-segment elevation (leads V1 through V3) on electrocardiogram and symptoms (cardiac syncope) or ventricular arrhythmia indicates the presence of Brugada syndrome.