MKSAP Quiz: Follow-up on ED visit
A 31-year-old man is evaluated for follow-up 2 days after an emergency department visit for palpitations. He reports intermittent palpitations and occasional episodes of shortness of breath. These episodes have increased in frequency and are often accompanied by light-headedness. He experienced loss of consciousness on one occasion. He does not have chest discomfort or jaw pain. His medical history is unremarkable except for a previous emergency department visit several years ago for palpitations. He has no significant family history.
On physical examination, the patient is afebrile, blood pressure is 105/68 mm Hg, pulse rate is 67/min, and respiration rate is 12/min. BMI is 24. His neck veins are flat, and the point of maximal impulse is in the midclavicular line without heave or lift. He has no lower extremity edema.
Serum thyroid-stimulating hormone level is normal.
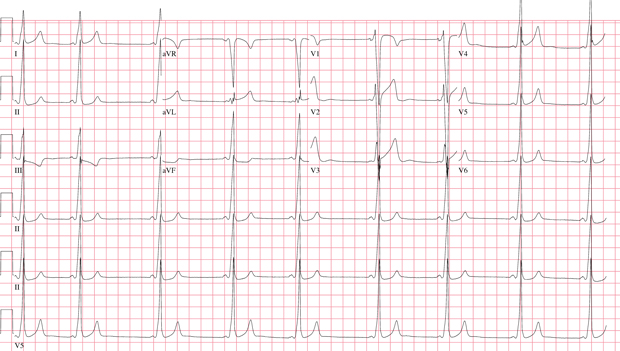
Electrocardiogram is shown. Transthoracic echocardiogram shows no structural abnormalities.
Which of the following is the most appropriate next step in management?
A. Antiarrhythmic drug therapy
B. Diltiazem
C. Electrophysiology study
D. Metoprolol
Answer and critique
The correct answer is C: Electrophysiology study. This question can be found in MKSAP 17 in the Cardiovascular Medicine section, item 115.
This patient should undergo an electrophysiology study. He has evidence of preexcitation on his electrocardiogram with a history of palpitations and syncope. The slurring of the QRS complex (delta wave) represents early ventricular depolarization owing to conduction over the accessory pathway (bypass tract). The presence of a delta wave and symptoms of tachycardia are consistent with Wolff-Parkinson-White syndrome. The episodes could be caused by supraventricular tachycardia (orthodromic or antidromic reciprocating tachycardia) or preexcited atrial fibrillation. The presence of syncope suggests that these episodes are hemodynamically significant. Identification of syncope in a patient with Wolff-Parkinson-White syndrome should prompt referral to a cardiologist or electrophysiologist.
An electrophysiology study would allow diagnosis of the cause of this patient's palpitations and allow risk stratification for risk of sudden cardiac death. The electrophysiology procedure also affords the opportunity to ablate the accessory pathway and potentially cure his arrhythmia. Stress testing can be an appropriate method for risk stratification in patients with asymptomatic preexcitation; however, this patient clearly has symptoms and therefore should undergo invasive testing and ablation.
Antiarrhythmic drug therapy is not indicated in this patient because the type and mechanism of the arrhythmia are not known. Catheter ablation is preferred in young persons with Wolff-Parkinson-White syndrome in order to avoid lifelong use of potentially toxic medications. Antiarrhythmic agents are reserved for second-line therapy, particularly in patients with accessory pathways located close to the atrioventricular (AV) node.
Metoprolol and diltiazem are AV nodal blockers and may be unsafe if the patient has anterograde conduction down the accessory pathway during atrial fibrillation. These drugs can block the AV node and promote rapid 1:1 conduction from the atrium to the ventricle during atrial fibrillation and thus induce ventricular fibrillation. AV nodal blockers are contraindicated in patients with preexcited atrial fibrillation, such as this patient.
Key Point
- Identification of syncope in a patient with preexcitation should prompt referral to a cardiologist or electrophysiologist.



