MKSAP Quiz: 3-week history of progressive fatigue
A 28-year-old previously healthy woman is evaluated in the hospital for a 3-week history of progressive fatigue, dyspnea with exertion, and easy bruisability.
On physical examination, temperature is 37.2°C (98.9°F), blood pressure is 124/78 mm Hg, pulse rate is 96/min, and respiration rate is 16/min. Oxygen saturation is 97% with the patient breathing ambient air. She has conjunctival pallor. Scattered petechiae are visible over the pretibial area as are ecchymoses on the upper extremities. Lymphadenopathy, consisting of 1.5- to 2.0-cm lymph nodes in the bilateral cervical, axillary, and inguinal lymph node chains, is found. Cardiopulmonary examination is normal. Hepatosplenomegaly is absent.
Laboratory studies:
| Hemoglobin: | 7.4 g/dL (74 g/L) |
| Absolute neutrophil count: | 400/µL (0.4 × 109/L) |
| Direct Coombs (antiglobulin) test: | Negative |
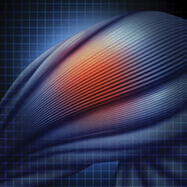
The prothrombin time and activated partial thromboplastin time as well as serum calcium, phosphorus, and potassium levels, are normal. A peripheral blood smear is shown.

A posteroanterior/lateral chest radiograph is normal.
A bone marrow aspirate and biopsy shows extensive infiltration with cells similar to those found on the peripheral blood smear. The cells are positive for CD34, CD10, CD20, and TdT. Cytogenetics are normal.
In addition to intravenous fluid hydration and allopurinol, which of the following is the most appropriate treatment?
A. Imatinib
B. Induction chemotherapy
C. Leukapheresis
D. Rituximab
Answer and critique
The correct answer is B: Induction chemotherapy. This question can be found in MKSAP 16 in the Hematology and Oncology section, item 51.
The most appropriate treatment is induction chemotherapy consisting of daunorubicin, vincristine, L-asparaginase, and prednisone. This patient meets the diagnostic criteria for B-cell acute lymphoblastic leukemia (ALL) with 25% lymphoblasts or more on bone marrow examination. The blasts can be identified as lymphoid because they are TdT-positive and because CD10 and CD20 are B-cell markers. Standard induction therapies vary, but an anthracycline agent plus vincristine, a corticosteroid, and L-asparaginase constitute the core for most regimens used today. Although complete remission rates with induction therapy are very high (>90%), relapse remains a problem. Higher-risk patients with a suitable donor are often considered for allogeneic stem cell transplantation during first remission.
Imatinib is a BCR-ABL inhibitor used for the treatment of chronic myeloid leukemia. It is used to treat Philadelphia chromosome-positive ALL, most commonly in combination with cytotoxic chemotherapy. However, because this patient's cytogenetics are normal, imatinib would not be appropriate.
Leukapheresis is not indicated. Although this patient has a high circulating blast count, she has no symptoms or signs of hyperleukocytosis, which is characterized by respiratory abnormalities, including dyspnea and diffuse interstitial and/or alveolar infiltrates on chest imaging, and neurologic symptoms consisting of dizziness, mental status changes, visual changes, headaches, and tinnitus. Furthermore, symptomatic hyperleukocytosis is more common in acute myeloid leukemia (AML) and rarely occurs in ALL. Lastly, the benefits of leukapheresis in the setting of symptomatic hyperleukocytosis remain unclear.
Although this patient's lymphoblasts are CD20-positive, the role of rituximab in the treatment of CD20-positive B-cell ALL is unproven.
Key Point
- Induction therapy consisting of combination chemotherapy constitutes the basis for most regimens used today to treat B-cell acute lymphoblastic leukemia.