MKSAP Quiz: ED evaluation for midsternal pain
A 59-year-old woman is evaluated in the emergency department for midsternal chest pain. The pain began several hours ago as a vague ache in her left upper sternal region that progressed in intensity and severity. The pain abated spontaneously after approximately 45 minutes. She had no further chest pain until several hours later, when it recurred unprovoked by exertion. She has no shortness of breath, nausea or vomiting, syncope, previous history of chest pain, or known cardiac disease or risk factors for venous thromboembolism. Medical history is significant for hyperlipidemia and hypertension. She does not smoke cigarettes. Medications are simvastatin, aspirin, lisinopril, and hydrochlorothiazide.
On physical examination, she is afebrile, blood pressure is 110/70 mm Hg, pulse rate is 68/min, and respiration rate is 22/min. BMI is 28. Oxygen saturation on ambient air is 97%. Estimated central venous pressure is 8 cm H2O and carotid pulses are without bruits. Lungs are clear. Heart sounds are normal. There is a grade 2/6 holosystolic murmur at the left sternal border with radiation to the apex. There is no lower-extremity edema. The remainder of the examination is normal.
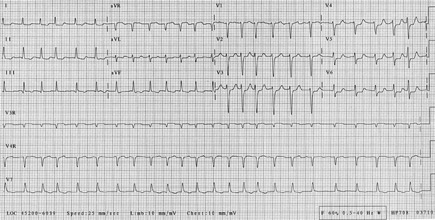
Electrocardiogram is shown. Chest radiograph is normal.
Which of the following is the most appropriate initial management of this patient?
A. Adenosine stress test
B. Admit to the coronary care unit
C. CT pulmonary angiography
D. Ibuprofen administration
Answer and critique
The correct answer is B: Admit to the coronary care unit. This question can be found in MKSAP 16 in the General Internal Medicine section, item 101.
This patient should be admitted to the coronary care unit for further treatment. Because chest pain is a common clinical symptom and may have noncardiac causes, assessment of the probability that chest pain has a cardiac etiology is critical to pursuing appropriate diagnosis and treatment. This is done through an understanding of existing cardiac risk factors, the nature of the presenting symptoms, findings on physical examination, and the results of specific initial diagnostic studies, such as chest radiography and electrocardiography. Her cardiac risk factors include her age, hypertension, and hyperlipidemia, and the substernal nature of her chest pain places her in an intermediate risk category for cardiac-related pain. Coupled with her electrocardiogram (ECG) showing anterolateral ST-segment depression, her clinical picture is consistent with coronary ischemia as the cause of her chest pain. She therefore requires emergent treatment for coronary ischemia and admission to a coronary care unit.
Low-risk patients without evidence of myocardial infarction can be evaluated with an exercise or pharmacologic stress test. However, a stress test in a patient with probable acute coronary syndrome could provoke an extension of her myocardial infarction or a life-threatening arrhythmia.
CT pulmonary angiography would be helpful if there were a high probability of acute pulmonary embolism. Because this patient has symptoms and ECG findings of acute coronary syndrome and the probability of pulmonary embolism is low (she has no risk factors or physical examination findings to support the diagnosis of venous thromboembolism and her symptoms can be explained by an alternative diagnosis), a CT pulmonary angiogram is not indicated.
NSAIDs are indicated for the treatment of acute pericarditis or musculoskeletal chest wall pain. The pain of pericarditis is characteristically pleuritic in nature. In addition, the characteristic ECG finding in pericarditis is ST-segment elevation throughout the precordial and limb leads rather than regional ST-segment depression, as in this patient. ECG changes are not present in musculoskeletal chest pain.
Key Point
- Assessment of chest pain is based on preexisting risks for cardiac or other diseases, elements of the history and physical examination, and appropriate, directed testing based on the likely cause of chest symptoms.





