MKSAP Quiz: 6-month history of dysphagia
A 50-year-old man is evaluated for a 6-month history of dysphagia. He describes a sensation of both solids and liquids sticking in the midesophageal area. This sensation has slowly worsened over time. He also describes intermittent midsternal discomfort that is nonexertional and is usually precipitated by swallowing food. He has lost 4.5 kg (10.0 lb). He has had no history of heartburn or acid regurgitation.
Physical examination is normal.
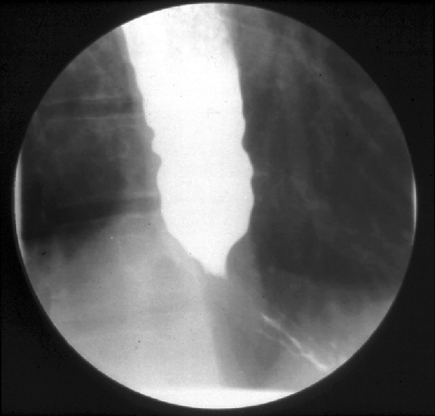
A barium swallow is shown. Esophageal manometry shows aperistalsis with swallowing of liquids.
Which of the following is the most appropriate management?
A. CT of the chest and abdomen
B. Endoscopy
C. Myotomy
D. Trial of swallowed aerosolized corticosteroids
Answer and critique
The correct answer is B: Endoscopy. This question can be found in MKSAP 16 in the Gastroenterology and Hepatology section, item 92.
The most appropriate next step in management is endoscopy. This patient's history (dysphagia to solids and liquids with intermittent chest pain) and evaluation (barium radiography showing a dilated esophagus with a smoothly tapering end [bird's beak]; esophageal manometry showing aperistalsis) are suggestive of achalasia. Achalasia, the best characterized of the esophageal motility disorders, consists of the failure of the lower esophageal sphincter to relax with swallowing. The resulting functional obstruction of the distal esophagus leads to dysphagia, chest pain, regurgitation of food, and weight loss. Achalasia is thought to be caused by degeneration of the myenteric plexus with resulting loss of inhibitory neurons in the lower esophageal sphincter, which remains tonically contracted. Owing to the relatively short history (6 months) and weight loss of 4.5 kg (10.0 lb), endoscopy should be performed to rule out a malignant mass at the gastroesophageal junction before considering therapeutic options. A malignant mass could be associated with nonrelaxation of the lower esophageal sphincter owing to direct malignant infiltration or a paraneoplastic syndrome (pseudoachalasia).
CT of the chest and abdomen might be indicated in a patient in whom a malignant mass is discovered at the gastroesophageal junction. Because most malignancies associated with pseudoachalasia are gastric adenocarcinomas, abdominal and chest CT examinations are usually performed for proper staging. Evidence of metastatic spread will spare the patient unnecessary surgery. However, it would be premature to pursue these diagnostic studies before endoscopy is performed.
Surgical disruption of the lower esophageal sphincter (myotomy) can be performed laparoscopically through the abdomen and is considered a first-line therapy for achalasia. However, performing the procedure before excluding the presence of tumor-related pseudoachalasia would be inappropriate.
Swallowed aerosolized corticosteroids would be indicated in the setting of eosinophilic esophagitis, which is unlikely in this patient owing to his barium radiograph and esophageal manometry findings.
Key Point
- Upper endoscopy should be performed to exclude mechanical obstruction of the esophagus in the region of the lower sphincter, particularly if there is concern for underlying malignancy (indicated by shorter duration of symptoms and rapid weight loss).