Early interventions overlooked in OA
Osteoarthritis has been somewhat neglected, according to a recently formed consortium that is advocating for more proactive diagnosis and intervention. Earlier screening and a less reactive approach might head off some of the worst of the difficulties and related treatment costs.
Compared with other high-profile chronic disease targets like diabetes or hypertension, osteoarthritis has been somewhat neglected, according to a recently formed consortium that's advocating for more proactive diagnosis and intervention.
Too frequently, doctors overlook the painful joint disease at a stage when preventive measures such as exercise and weight loss could be most beneficial, said physicians involved with the Chronic Osteoarthritis Management Initiative (COAMI).
Earlier screening and a less reactive approach might head off some of the worst of the functioning difficulties and related treatment costs, said Angela McLean, MD, ACP Member, who serves as the initiative's ACP representative.
“Frequently you will get that individual who comes in with severe osteoarthritis and is basically ready for a knee replacement,” said Dr. McLean, an associate professor of medicine at Louisiana State University School of Medicine in New Orleans. “There may have been things that we could have done earlier on to prevent rapid progression, so that maybe you could delay or prevent the need for replacement.”
Osteoarthritis damages the joints of an estimated 27 million Americans, according to a frequently cited 2008 study in Arthritis & Rheumatism. Yet treatment options for osteoarthritis continue to remain limited, compared with the advances in disease-modifying drugs for its counterpart, rheumatoid arthritis.
Meanwhile, diagnoses for osteoarthritis and other chronic conditions are likely to continue to accelerate in an aging and increasingly overweight American population. A heftier body mass index can weigh down vulnerable joints. Conversely, painful joints make it more difficult for aging adults to stay mobile, which is vital to preventing diabetes, hypertension and other conditions.
COAMI is part of the United States Bone and Joint Initiative, a collaboration of more than 100 health-related organizations, and held its first work group meeting in 2012. Also in 2012, the American College of Rheumatology (ACR) released an updated set of guidelines on osteoarthritis, its first since 2000, which highlight the value of trying exercise and weight loss first, whenever feasible, said Marc Hochberg, MD, MPH, FACP.
“The new [research] data supports and extends the efficacy in terms of improvement in pain and improvement in function,” said Dr. Hochberg, lead author of ACR's guidelines, which were published in Arthritis Care & Research, and a professor of medicine, epidemiology and public health at the University of Maryland School of Medicine in Baltimore. “And it stresses the fact that they should be combined together—that you get a synergistic effect with exercise and weight loss.”
Earlier screening
According to data from the Centers for Disease Control and Prevention published in 2010 in the Morbidity and Mortality Weekly Report, 22.2% of Americans reported that a doctor had diagnosed them with some form of arthritis. And arthritis risk rises as aging Americans pack on the pounds, according to a battery of studies cited in the COAMI work group report, which was released in September 2012.
By age 85, 44.7% of Americans will have knee osteoarthritis symptoms, according to a 2008 study published in Arthritis & Rheumatism. But the risk is far greater for the heaviest individuals, with 60.5% of obese Americans symptomatic compared with 30.2% of normal-weight individuals.
The last-ditch option of a knee or hip replacement is pricey. In 2009, the United States spent $42.3 billion on a total of 905,000 such replacements, mostly related to osteoarthritis, according to data from the COAMI report based on federal statistics.
Moving forward, one of the initiative's goals is to develop an assessment tool, similar to the FRAX tool used to assess osteoporotic fracture risk, to monitor the extent and impact of osteoarthritis as patients age, Dr. McLean said.
In the meantime, she recommends that physicians incorporate a few questions into routine checkups, perhaps starting as early as college or graduate school physicals, to get a snapshot of potential osteoarthritis risk. For example, young adults can be asked if a family member has needed a joint replacement, she said. They also can be asked about any prior traumatic injury to one of their joints, which can heighten their vulnerability to later osteoarthritis.
If such an injury is identified, exercises can be recommended to strengthen the surrounding muscles, Dr. McLean said. With younger overweight or obese patients, the primary care doctor can add osteoarthritis to the list of health risks they face if they don't take steps to lighten up, she said.
Primary care doctors also should keep in mind that other medical conditions can foster the emergence of osteoarthritis in later years, said Bernard Rubin, DO, MPH, FACP, division head of rheumatology at the Henry Ford Health System in Detroit.
Patients with diabetes might develop secondary osteoarthritis, sometimes due to the peripheral neuropathy that can impact sensations in their feet and thus related body mechanics, he said. Spinal changes, such as those caused by scoliosis, can similarly place joints at risk.
Proactive diagnosis
With numerous possible types of arthritis, it can sometimes be difficult to identify early osteoarthritis specifically, said Sharon Kolasinski, MD, FACP, professor of medicine at the Cooper Medical School of Rowan University in Camden, N.J.

One possible scenario: A woman walks into the office reporting hand pain. Osteoarthritis and rheumatoid arthritis are two likely possibilities, but a more detailed exam and history will be needed to try to differentiate which one, Dr. Kolasinski said.
Some symptoms, such as joint stiffness upon waking, particularly if it extends longer than an hour, are more likely to be rheumatoid arthritis, Dr. Kolasinski said. Sometimes, the location of discomfort can point to a diagnosis, she said. Osteoarthritis of the hand is more likely to develop in one of several joints, including where the thumb meets the wrist, or in the middle joints of the fingers or those joints nearest the tips.
By palpating painful joints, doctors might be able to identify rheumatoid arthritis-like swelling. But even experienced physicians can sometimes struggle to identify swollen versus enlarged joints, Dr. Kolasinski said, echoing a point made by others.
When uncertainty persists, drawing a patient's blood to test for rheumatoid factor won't sort out the mystery, Dr. Rubin said. As people age, they are more likely to test positive, even when the underlying cause isn't rheumatoid arthritis, he said.
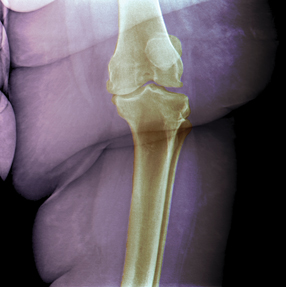
But an X-ray can reveal the bony growths associated with osteoarthritis, Drs. Kolasinski and Rubin said. “The X-ray difference between osteoarthritis and rheumatoid arthritis is striking,” Dr. Rubin said. “So that would be very, very useful.”
Some basic legwork during the physical exam also can provide the physician a window into the extent of the patient's discomfort and functional difficulties, Dr. Rubin said. Talking to a patient sitting in an exam room chair isn't illuminating, he said.
“You've never watched the patient move from point A to point B,” he said. “You've never watched the patient get up out of a chair. You don't know if they use a cane, if they use it correctly or is it the right height?”
Instead, walk with the patient a few steps down the hallway, perhaps while talking about other health issues that need to be addressed, Dr. Rubin said. “While you are talking to them, and you might be holding their arm, you might be gaining a lot of information,” he said.
Earlier intervention
For diagnoses of knee or hip osteoarthritis, convincing a patient to lose extra weight and get moving should be the first line of treatment, according to arthritis experts.
The nurse or physician assistant in the primary care doctor's office might be able to handle whatever nutritional counseling can encourage weight loss, Dr. Hochberg said. But he stressed that getting a physical therapist involved is key to a patient's success when it comes to improving exercise and mobility.
A physical therapist can perform an individualized evaluation to identify what sort of exercise poses less risk for a patient's joints and fits with his or her personality and lifestyle preferences, Dr. Hochberg said. “They are more likely to be adherent if they're doing something they like doing,” he said. “Some people like swimming. Other people don't want to get into a pool.”
Even seemingly small amounts of weight loss can take a much larger burden off the joints, according to a 2005 study published in Arthritis & Rheumatism. The study assessed the joint load for 142 overweight and obese older adults and found that each pound lost translated to a fourfold lighter load on the adults' knee joints.
Drug management
By postponing the more severe symptoms of osteoarthritis, patients can at least temporarily avoid more aggressive treatment options, which have various drawbacks, arthritis experts said.
Doctors have been moving away from using opioids unless absolutely necessary, leaving relatively few medication classes other than acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), Dr. McLean said.
In addition, surgery has its inherent limits, since the lifespan of a replacement is typically 10 to 15 years, and after that a second surgery might be needed, said Matthew Beal, MD, assistant professor of clinical orthopedics at Ohio State University Wexner Medical Center in Columbus.
Given worries about liver toxicity, the role of acetaminophen is downplayed in the most recent ACR guidelines; it is recommended as only one of the first-line medication options, Dr. Hochberg said. The guidelines also state that a doctor prescribing the maximum dose of 4 g daily should counsel the patient to steer clear of any other acetaminophen-containing product, including nonprescription cold medicines.
In selecting a medication to prescribe, though, primary care doctors should not be quick to dismiss NSAIDs as an option, despite heart-related effects that emerged over the last decade, beginning with cyclooxygenase-2 inhibitors such as rofecoxib (Vioxx), Dr. Hochberg said. Some think the pendulum against using NSAIDs has swung too far in the other direction, he said, “that NSAIDs are being avoided even in people who are not at increased risk.”
The extent of the patient's heart-related risk should be assessed when making prescribing decisions, Dr. Hochberg said. While it's wise to avoid NSAIDs for someone who previously had a heart attack, doctors shouldn't as quickly rule them out for patients with diabetes, hypertension or other heart risk factors, particularly if they're being successfully treated, he said.
The guidelines also conditionally recommend against the use of two popular alternative remedies, glucosamine and chondroitin sulfate, citing mixed results in several studies since 2000. For example, one 2010 BMJ meta-analysis cited by the guidelines assessed 10 studies involving 3,803 patients. It found that neither glucosamine nor chondroitin separately or the two combined reduced pain or joint-space narrowing in patients with knee or hip osteoarthritis compared with placebo.
Narcotics and surgery
For patients living with severe knee or hip osteoarthritis and experiencing limited relief from non-narcotic drugs, the next logical step would be to refer them to a surgeon to discuss a possible joint replacement, Dr. Hochberg said.
That option should be pursued before an opioid is prescribed, he said. Only if the patient refuses surgery or is not a good candidate due to other medical issues should narcotic drugs be tried, he said. (In that event, Dr. Hochberg recommends that the patient be referred to a rheumatologist.) The ACR guidelines also suggest that physicians looking for opioid guidance consult the 2009 chronic pain guidelines developed by the American Pain Society and American Academy of Pain Medicine.
Along with their potential addictive properties, opioids also have been shown to boost the fracture risk in older patients, Dr. Hochberg said. He cited one study published in 2010 in Archives of Internal Medicine, which found that Medicare patients with a mean age of 80 years were more likely to experience a fracture while taking an opioid versus an NSAID.
While the decision to get a joint replacement is highly personal, a key factor is the degree to which patients' joint pain is impacting their daily functioning or their personal safety, said Dr. Beal, Ohio State's orthopedic surgeon. Has a patient developed workarounds that slow her down, such as avoiding the stairs or leaning on the kitchen counters for support?
Another red flag is if a patient admits to occasionally being unstable on his or her feet. “That's a great question to ask because that's usually a sign of progression of arthritis,” Dr. Beal said.
But don't refer patients for a surgical consult if they are highly resistant, Dr. Beal said. In some cases, he said, severe damage can be visible on an X-ray but patients say they are coping just fine. “It's a quality-of-life question,” he said. “Are you able to do what you want to do?”
Plus, he added, “There are some patients that can't mentally swallow the idea of going to surgery. Sometimes it's not so much that the primary care folks are waiting [to make the surgical referral]. It's that the patient is not really ready to have that discussion.”




