Hopes and fears abound at National Bundled Payment Summit
Expansion of bundled payments to chronic disease treatment for internists would be complicated, but it's garnering interest. Demonstration projects show that hospitals that reduced the cost of care were able to pay physicians up to an extra 25% of what they would normally earn for their services.
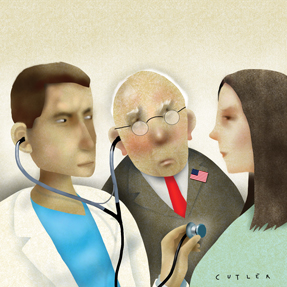
Bundled payments are going to be fun, according to Paul Ginsburg, president of the Center for Studying Health System Change. “If you're a provider and you're at risk, I'm sure you're going to be sweating,” he told attendees at the first-ever National Bundled Payment Summit. “But think of the consultants.”
Joking aside, speakers at the summit, held in Washington, D.C., last October, were optimistic about the potential for this alternative payment model to reduce health care costs without decreasing profits for hospitals or physicians.

Much of the discussion focused on the Center for Medicare and Medicaid Innovation's (CMMI) call for hospitals and physician groups to experiment with bundled payment models. At the time of the conference, the CMMI had proposed four possible models for pilot programs, and four more were expected soon. The models differ in their payment specifics and their inclusion of acute care, post-acute care or both settings, but the common focus is on combining physician and hospital billing into a single Medicare charge to motivate physicians and hospitals to reduce costs.
Even at this early point (the agency is still collecting applications for the pilots) the models are attracting interest, according to Valinda Rutledge, director of the care models group at CMMI. “The response was incredible” to the agency's request for letters of intent from interested participants, she noted.
Experts said the enthusiasm represents a significant change from the response to another recent attempt at payment restructuring, accountable care organizations. “ACO regulations were received with a big thud,” said Robert A. Minkin, senior vice president of The Camden Group, a health care consulting company.
But he sees more potential for action with the bundled payments pilots, which could be a stepping stone to larger accountable care projects. “It is a fundamental game changer from the old rules. All of those things that make our hospitals financially successful have been turned on their heads,” he said. Mr. Minkin got a preview of the effects of bundled payment in his work with St. Joseph Hospital in Denver, one of the participants in Medicare's Acute Care Episode (ACE) demonstration.
Under the ACE program, participating hospitals received a pre-set combined payment for Medicare Part A and Part B services for some specified cardiovascular and orthopedic procedures. The ACE demonstration contained many components included also in the CMMI pilots and provided a preview of the changes in physician and hospital practices that will be required, Mr. Minkin noted. “Physicians have to engage differently,” he said.
Development of protocols was a major way that physicians contributed to the demonstration at St. Joseph. “You have to find ways to lower risk and cost. Get the variations down to zero,” said Mr. Minkin. “Every hospital has two or three guys who do it best.” Those physicians who provide high quality for low cost should be the models for their colleagues and hospital protocols, he said.
Efforts in this direction at St. Joseph did create some conflict, according to Deirdre Baggot, RN, vice president with The Camden Group. Not all physicians were eager to engage in a program reaching throughout, and even outside, the hospital to cut costs. “I didn't go to medical school to take responsibility for readmissions,” responded some physicians, according to Ms. Baggot.
But there are advantages for doctors who do buy into the bundled payment system. The ACE demonstration project allowed hospitals that reduced the cost of care to share the savings with participating physicians, up to an extra 25% of what they would normally earn for their services.
Some of the new models increase that gainsharing to 50%. “Your participating physicians may be able to earn more money for the same procedures without any additional work,” said Bill Phillips, a consultant from Ft. Lauderdale, Fla.
As his statement implies, most bundled payment programs thus far have focused on procedure-related hospitalizations, such as knee and hip replacements or coronary artery bypass. In general, bundled payments will make the most sense for the types of hospitalizations that are associated with widely varying costs, according to Mr. Ginsburg. “If you see large variation in resources used or quality from institution to institution, it points to opportunities to do better,” he said.
Treatments that entail expensive devices are also a likely target for savings, according to Nancy G. Harrison, director of the ACE project at Ardent Health Services in Nashville, Tenn. Her hospital not only educated physicians about the costs of their supplies, such as stents, but also took the physicians into meetings with vendors to negotiate discounts. “The vendor saw that the physician was ready to change [suppliers]. They do not want to lose that market share,” said Ms. Harrison.
Expansion of bundled payments to the chronic disease treatment that more often involves internists is “on our radar,” according to Ms. Rutledge of CMMI. “We have heard from individuals around the country that they'd like us to do a chronic care bundle,” she said. Decisions about how much time and how many clinicians to include in such bundles would be more complicated, however, the experts noted.
The agency is also struggling with how to get patients involved in bundled payments. The ACE demonstrations included rebates to patients when their hospitalizations resulted in savings to Medicare, a feature that has not been included in the new CMMI models. The checks did not seem to be having the desired effect on patients, some of whom responded with such statements as “Is it not a good hospital because it's less money?” Ms. Rutledge reported.
Finding an effective way to interest patients in cost-consciousness and hospital choice will be key to the success of bundled payments, according to several speakers at the conference. Prior failures contributed to the lack of success of managed care programs, according to Stuart Altman, PhD, professor of health policy at Brandeis University in Waltham, Mass. “Patients felt that all the savings of managed care were going to employers and insurers....If they feel that the government is saving money and they're not, the backlash is going to continue,” he said. “They have to see the benefits and the costs of going to one institution and not another.”
This is only one of a number of issues yet to be worked out with bundled payments, experts said. There's the risk that the system could work out too well for providers. “Medicare's fear is that they're going to wake up next year and read a headline, ‘Hospitals report record profits thanks to accountable care organizations and bundled payments,’” said Harold Miller, executive director of the Center for Healthcare Quality and Payment Reform, a Pittsburgh-based advocacy organization.
Too much profit for pilot participants could also drive change in the wrong direction. “If the bundles make it more lucrative, I think people will start looking at how they can do more of these episodes,” said Mr. Miller.
Or, conversely, the programs could fail to motivate any change. CMMI models one, two and three involve retrospective payment plans, in which Medicare will pay in the usual fee-for-service system and then issue bonuses or penalties based on how the payments compare to target prices for the bundle of care.
Mr. Ginsburg described this as “virtual” bundled payments and argued that a prospective system, which the fourth CMMI model has, would be more effective at encouraging and funding coordination of care. “Real bundled payment has a much greater upside. This way providers can actually start to work together,” he said. Mr. Minkin also recommended against continuing fee-for-service payments, suggesting hospitals set their contracts at physicians' current level of income, with the potential for bonuses from savings, to remove the incentive to perform more procedures.
But really cutting health care costs may take more than incentives, according to Mr. Ginsburg. Medicare has the authority to make the bundled payment pilots permanent, but legislation would be required to make them mandatory. “If there's going to be a substantial effect on spending, they probably need to be mandatory,” he said.
Ms. Rutledge didn't address that possibility, but she did say that Medicare would be keeping a close eye on the success or failure of the bundled payment experiment and acting quickly on the findings. “We have to figure out how to make a business case that's sustainable. If we find out that one of the awardees' (pilot programs) is doing incredible, we will make sure that all the other awardees are aware of it,” she said.