Seeing the whole diagnostic picture
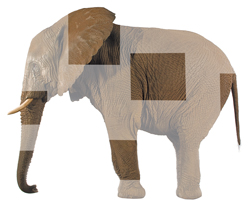
For a year, one patient saw specialist after specialist and received a different diagnosis each time. Like the story of the blind men and the elephant, specialists often see the patient through only one component of training, as anchoring and availability sneak into their thinking.
Susan Sorensen, FACP, an internist and hematologist in Palo Alto, Calif., told us of a case where the correct diagnosis took more than a year to make. The patient was a 24-year-old woman who had developed weight loss, fatigue and intermittent chest tightness. She was seen in a local emergency department, and was told that she should consult a pulmonary specialist. A chest X-ray and EKG appeared normal.
Over the next few months, she continued to feel unwell, losing more weight and developing a new symptom, intermittent abdominal pain, predominantly in her left lower quadrant. She was seen again in the emergency department, and received a diagnosis of possible urinary tract infection. A course of antibiotics did not improve her symptoms. She returned to the emergency department during a bout of abdominal pain, and was referred to a gynecologist. A pelvic ultrasound was unremarkable, and she was prescribed a second course of antibiotics for possible pelvic inflammatory disease.
She did not improve after this second empiric regimen of antibiotics, and continued to experience intermittent symptoms of abdominal pain, mostly in the left lower quadrant, with frequent bowel movements but no diarrhea. She lost an additional 10 pounds, and noted early satiety. After another visit to the emergency department, she was referred to a gastroenterologist, who evaluated her for celiac disease and tested her for food allergies; all tests were negative. The gastroenterologist performed an upper endoscopy, which was unremarkable.
Her symptoms persisted and she developed drenching night sweats and excruciating headaches, which prompted another visit to the emergency department. Neurological evaluation, including an MRI scan of the head and an EEG, were negative. She was given the diagnosis of possible abdominal migraine. An endocrine evaluation yielded a normal corticotropin stimulation test. A bout of severe nausea brought her once again to the emergency department and she was treated with ondansetron (Zofran). The emergency department physician noted cervical lymphadenopathy and she was referred for a lymph node aspiration, which yielded only adipose tissue. A workup for a possible occult malignancy, including a CT scan of the chest, abdomen, and pelvis, was negative, although sclerosis of the sacroiliac joints was noted. Lacking a diagnosis, a house officer told her, “You need to eat more.”
An internist steps in
After more than six visits to the emergency department and evaluations by multiple specialists, the patient was referred to Dr. Sorensen.
The first thing the woman said was, “I am afraid I'm wasting your time. I am not having any pain right now.” Dr. Sorensen realized that the patient thought it was only appropriate to seek help for her symptoms when she was having an acute episode. Each time she received care in an emergency department, and then was referred to a different specialist. Her symptoms had now been present for almost a year, and included drenching night sweats, bowel movements after each meal, nausea, anorexia and abdominal pain that was intermittent and most prominent in the left lower quadrant.
On further questioning, she reported left hip stiffness and right knee pain. Her medical history was significant for seronegative juvenile rheumatoid arthritis as a child, which had resolved at puberty. A 17-year-old cousin had recently been diagnosed with Crohn's disease.
On physical exam, her body mass index was 16.8. There was mild tenderness in the left lower quadrant and, on pelvic examination, tenderness in the left adnexa. Her left sacroiliac joint was quite tender to palpation. Additional laboratory testing included negative antinuclear antibody panel and negative stool cultures. Dr Sorensen reviewed all of the patient's previous scans and confirmed the presence of sacroiliitis. Her human leukocyte antigen B27 was negative.
Dr. Sorensen suspected a diagnosis of Crohn's disease, and this was confirmed with lower endoscopy and biopsy of the terminal ileum. The patient was treated with mesalamine with improvement of her symptoms.
Through a lens, narrowly
As we heard this case, we were reminded of the parable of the blind men and the elephant. There are versions of this tale in many cultures, each slightly different, but the most famous one is the Hindi version popularized by John Godfrey Saxe in his poem. A group of blind men touch an elephant to determine what it is like. Each one touches only one part of the elephant, and they then can't agree. In the case of this young woman, each specialist viewed the patient's symptoms in the context of his or her own specialty.
Each saw the patient's problems through a narrow lens, and demonstrated a mix of anchoring and availability. Anchoring is seizing upon the first bit of information that you encounter, analogous to grasping the elephant's tail or its tusk or its leg. Availability is calling up what is most familiar or dramatic in past encounters, and understandably, specialists think about diagnoses within their own field, because they are most experienced with these disorders and they consider them first. Indeed, as the case unfolded, each of us immediately thought of diagnoses in our own disciplines: malignancy as an oncologist (Dr. Groopman), adrenal insufficiency or hyperthyroidism as an endocrinologist (Dr. Hartzband).
It is particularly the role of the internist to consider the disparate fragments of the patient's history, examination and evaluation and knit these pieces together to arrive at the correct diagnosis, mindful that each isolated part of the “elephant” must be combined with the others to yield the correct form.