MKSAP Quiz: Dyspnea during walking
A 79-year-old woman is seen for an annual examination. She is in good health except for osteopenia, for which she takes calcium and Vitamin D supplements. She walks regularly to and from the bus stop several times per week. It takes her 25 minutes to get to the bus stop whereas it only took her 10 minutes a year ago. She describes dyspnea midway in her walk, causing her to stop and catch her breath. She denies angina, presyncope, syncope, or pedal edema.
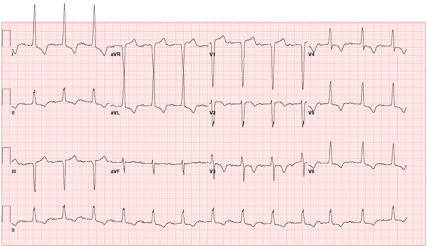
Physical examination shows a heart rate of 80/min and blood pressure of 165/86 mm Hg. Lungs are clear to auscultation. Carotid artery upstrokes are delayed. There is a sustained apical impulse. S1 is normal and there is a single S2 and an S4. A grade 3/6 late-peaking systolic murmur is heard best at the right 2nd intercostal space, with radiation into the right carotid artery. An electrocardiogram is shown. Transthoracic echocardiogram shows concentric left ventricular hypertrophy. The ejection fraction is 69% with no regional wall motion abnormalities. There is a trileaflet aortic valve with heavy calcification, an aortic jet velocity of 4.8 m/s, a peak transaortic gradient of 92 mm Hg, and a valve area of 0.7 cm2.
Which is the most appropriate option for improving this patient's quality of life?
A. Begin an angiotensin-converting enzyme inhibitor
B. Percutaneous aortic balloon valvuloplasty
C. Aortic valve replacement
D. A supervised cardiac exercise program
E. Discontinue calcium supplementation
Answer and critique
The correct answer is C) Aortic valve replacement. This question can be found in MKSAP 14 in the Cardiovascular section, Item 106.
This patient has echocardiographic criteria consistent with severe aortic stenosis. The most common cause of aortic stenosis is progressive calcific valve disease of a normal trileaflet valve. The primary indication for aortic valve replacement in patients with aortic stenosis is onset of cardiac symptoms. This patient has symptomatic disease with exertional dyspnea and decreased exercise tolerance. Referral for aortic valve replacement should be the next step in her management.
The initial compensatory mechanism for aortic stenosis is myocardial hypertrophy with preservation of systolic function. In this patient, there is evidence of left ventricular hypertrophy on the echocardiogram, also evidenced by characteristic changes on the electrocardiogram with a “strain” pattern. Although the classically taught symptoms of severe aortic stenosis are angina, congestive heart failure, and syncope, most patients initially present with more subtle symptoms, such as decreased exercise tolerance.
Previous studies have documented a postoperative survival and return to quality of life status in patients with aortic stenosis following aortic valve replacement that is nearly normalized to that of age-matched individuals without aortic stenosis. Older patients may be inclined to refuse valve replacement due to the perceived risks of surgery, but should be educated that both long-term survival and overall quality of life will be improved if aortic valve replacement is performed. This patient should not be refused surgery based on her age.
In general, medical management alone is not indicated in symptomatic aortic stenosis patients given the dismal prognosis if valve replacement is delayed. In a study of symptomatic patients with aortic stenosis who refused surgery, average survival was only 2 years, with a 5-year survival of less than 20%. In contrast, prognosis in patients with asymptomatic disease is excellent. Therefore, current guidelines drafted by the American College of Cardiology/American Heart Association advocate aortic valve replacement only once cardiac symptoms are present. Prophylactic aortic valve replacement in asymptomatic patients is not routinely performed due to the increased surgical risk, with complications such as thromboembolism, bleeding from anticoagulation, prosthetic valve dysfunction, and endocarditis.
Angiotensin-converting enzyme inhibitors are relatively contraindicated in the setting of significant aortic stenosis because afterload reduction may increase the effective pressure gradient across the stenotic aortic valve. Percutaneous aortic balloon valvuloplasty may initially provide a modest decrease in the outflow gradient, but there is often significant residual obstruction from leaflet thickening and annular calcification, recurrent stenosis typically occurs within months, and clinical trials to date have not demonstrated a beneficial effect on long-term outcome. Initiating a supervised cardiac exercise program is a useful adjunct to improve exercise tolerance in patients that are debilitated or deconditioned. This patient has symptomatic aortic stenosis, and a cardiac exercise program will not change her valvular hemodynamic parameters or cardiopulmonary symptoms preoperatively. A supervised cardiac exercise program would, however, be indicated following aortic valve replacement to limit postoperative deconditioning. Oral calcium supplementation does not accelerate the progression of valvular calcification; therefore, calcium therapy should not be discontinued.
Key Points
- Aortic valve replacement is recommended once symptom onset occurs, regardless of patient age.
- Symptom onset in aortic stenosis is often insidious and may include exertional dyspnea.





