MKSAP Quiz: preoperative evaluation for renal transplant
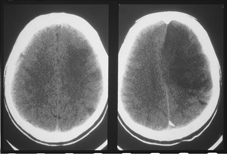
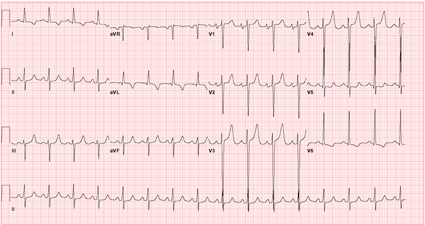
A 35-year-old man with a 20-year history of type 1 diabetes mellitus is undergoing preoperative evaluation for renal transplantation. His clinical course has been complicated by hypertension, diabetic retinopathy, and peripheral neuropathy that limits his ability to walk. His blood pressure is 142/85 mm Hg. His LDL cholesterol is 140 mg/dL (3.62 mmol/L) and his HDL cholesterol is 30 mg/dL (0.78 mmol/L). He currently smokes a half of a pack of cigarettes daily. His electrocardiogram is shown. Medical consultation is requested for evaluation of his preoperative cardiovascular risk.
Which of the following is the most appropriate recommendation at this time?
A. No further evaluation is needed
B. Serum C-reactive protein level
C. 24-hour electrocardiographic monitoring
D. Pharmacologic stress nuclear study
E. Coronary angiography
Answer and critique
The correct answer is D. Pharmacologic stress nuclear study.
In this patient with diabetes, dyslipidemia, smoking and hypertension, the Framingham 10-year likelihood of a cardiac event is 18%, compared to an average event rate of 5% for men of this age. In addition, diabetic patients frequently do not have angina despite the presence of ischemia (silent ischemia). This patient's electrocardiogram is consistent with left ventricular hypertrophy, based on an S wave in lead V2 plus an R wave in lead V6 > 35 mV, left axis deviation, and lateral ST-T changes. Left atrial enlargement also is present. Because the transplant team would defer transplantation until after coronary revascularization if significant disease were present, further evaluation is needed. A pharmacologic stress nuclear study is an appropriate diagnostic approach that provides information on the presence and severity of coronary ischemia. Exercise electrocardiographic stress testing would be less useful in this patient because his ability to exercise could be limited by peripheral neuropathy; in addition, the baseline electrocardiogram would likely show resting ST-segment changes due to left ventricular hypertrophy. Serum C-reactive protein levels are a marker of systemic inflammation, and population-based studies have demonstrated that elevated levels are associated with an increased risk of coronary disease. However, C-reactive protein levels are not helpful in detection of inducible ischemia in an individual patient. Although a 24-hour electrocardiogram could show ST-segment changes in a patient with silent ischemia, this approach is less sensitive and specific than stress testing, and its value would be limited in this patient with an abnormal resting electrocardiogram. Coronary angiography provides definitive evaluation of coronary anatomy and would likely demonstrate coronary artery disease in this patient. However, most clinicians would perform a stress imaging study first, both for diagnosis and to target which vessel should be considered for revascularization if multiple lesions are present.
Key points
- The risk of coronary artery disease in diabetic patients is two to four times higher than in nondiabetic patients.
- The pretest likelihood of disease should be calculated using available algorithms in patients with coronary risk factors.