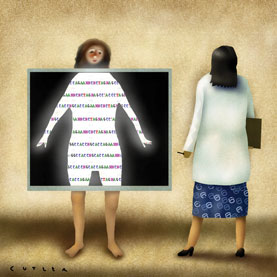
Genomics impacts everyday practices in unexpected ways
The hospitalization of a relative sets a leader in genomic research musing about how far medical practice has advanced in treating a common condition, and how far cutting-edge advances could go.
There is ongoing debate whether genomics will revolutionize medicine or if it's simply a pipe dream. From within the bubble of the National Institutes of Health, I at times wonder whether genomics has much of an effect outside of rare conditions and early adopter institutions.
Genomics and “personalized medicine,” as it has come to be known, are clearly changing care delivered by cutting-edge health care systems. For example, a major academic teaching hospital recently announced plans to offer tumor genomic profiling to all cancer patients. It's a nice benefit for those that land at such a hospital and can afford the estimated $2,000, but is there really much intersection with rank-and-file community hospitals or for bread-and-butter primary care diagnosis?

The recent hospitalization of a relative gives me confidence that we are, indeed, taking small steps toward genuinely personalized medicine. In May, my relative was admitted to a rural community hospital for atypical chest pain. The patient had no known risk factors for hypercoaguability save age, but was found to have lower extremity thrombus and bilateral pulmonary emboli (PE). The chest CT that picked up the PE also identified a 2 cm cystic pancreatic mass thought to represent an intraductal papillary mucinous neoplasm.
Over the next several days the patient's care intersected with genomic medicine three times, each illustrating pharmacogenetic, predictive and prognostic genetic testing.
First, the patient started on warfarin as long-term preventive therapy for recurrent PE. Currently, FDA-mandated warfarin labeling suggests health care providers consider pharmacogenetic testing to guide dosing. Simultaneous to the patient's admission, Medicare issued a provisional statement recommending that warfarin pharmacogenetic testing be covered in the setting of research trials designed to look at health outcomes. The patient wasn't tested, but it was considered.
Second, the patient's primary care hospital team ordered testing for a source of his apparent hypercoaguability, including tests for the Factor V Leiden and prothrombin gene mutations. The results from these tests testing help to explain potential causal factors and bear on predicting future disease risk (deep vein thrombosis and PE) for the patient and his family. In his case mutation testing was negative, so treatment decisions were based on empiric risk.
Finally, the patient's gastroenterologist ordered an endoscopy and fine needle aspiration of the cyst. The patient was informed that the aspirate would be subjected to a series of tests, one of which is a state-of-the-art molecular diagnostic assay for K-RAS mutations. Such testing, which falls somewhere between prognostic and diagnostic, has been shown to aid in differentiating benign vs. malignant tumors, a key to downstream tumor management (resection vs. observation). Little more than a decade ago these genomic tests would have been considered exotic if available at all outside of a major tertiary care setting. New discoveries coupled with mounting evidence of clinical benefit, though not necessarily from large randomized control type trials, has contributed to the increasing availability and insurance coverage of these applications.
While my relative benefited from cutting-edge care, the benefits were mitigated by a health care system that often works against itself. The patient spent three extra days in the hospital because under Medicare, insurance would not cover injectable low molecular weight heparin given in an outpatient setting. This directly cost the health care system a substantial sum simply because the pocket paying for an acute stay isn't connected to the pocket that pays for outpatient therapy with heparin. Indirectly, the prolonged admission diminished hospital system capacity, and exposed the patient needlessly to three additional days of possible hospital-induced iatrogenic harm.
My relative's admission for a PE to a rural community hospital illustrates how, with little fanfare, genomics and personalized medicine are suffusing into the practice of medicine. Likely none of the individual care-givers even realized that they had delivered personalized medicine. Rather they provided the personalized care that good clinicians have always strived to deliver.
Those in primary care who have questioned whether genomics is having much of an effect should take notice of this case. The benefits arrive daily, in small, often unexpected, steps and not necessarily in great leaps. It is time for all levels of medical education to provide the grounding in genomics that physicians will need to practice in the coming decades.
W. Gregory Feero, MD, PhD, a family physician with a doctorate in human genetics, is senior advisor for genomic medicine in the Office of the Director at the NIH's National Human Genomic Research Institute.