Barrett's esophagus: screening guidelines are in flux over reflux
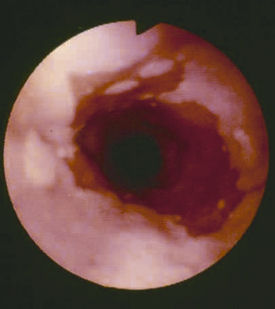
Barrett's esophagus, which is associated with chronic gastroesophageal reflux disease and is sometimes a precursor to cancer.
Barrett's esophagus, which is associated with chronic gastroesophageal reflux disease (GERD) and is sometimes a precursor to cancer, presents a diagnostic dilemma for many physicians. Only about 10% of patients with chronic GERD develop Barrett's esophagus, but an estimated 20% of U.S. adults have symptoms of heartburn at least once a week, too many to justify routine endoscopy.
But, the risk of developing cancer even when a patient has Barrett's esophagus is tiny, less than 1 percent a year. And experts disagree about whether screening will reduce mortality. The difficult clinical question becomes how should physicians sort through the large numbers of patients with heartburn and identify the small percentage who may have Barrett's esophagus or the even smaller numbers that may be at risk for adenocarcinomas?
“You are dealing with a phenomenon of a needle in a haystack, said Prateek Sharma, FACP, professor of medicine and gastroenterology at the University of Kansas School of Medicine. “It's a very important message to give patients that not everybody with heartburn or with Barrett's will end up getting cancer.” Dr. Sharma is the editorial consultant for ACP's Physician's Information and Education Resource (PIER) module on Barrett's esophagus.
Whether or not Barrett's screening occurs, experts agree that internists should take heartburn seriously and treat their patients with persistent symptoms of GERD with antacid medications more aggressively than they do now, particularly prescribing proton-pump inhibitors (PPIs). At the very least, these medications relieve patients' symptoms despite the lack of evidence they prevent Barrett's.
Screening and surveillance
The most recent guidelines on Barrett's esophagus published by the American College of Gastroenterology (ACG) in 2002 recommended screening once a wide population of patients with symptoms of heartburn. “Patients with chronic GERD symptoms,” the guidelines state, “are those most likely to have Barrett's esophagus and should undergo upper endoscopy.”
Based on subsequent evidence, many experts have come to identify “Caucasian men over age 50 with trunkal obesity (apple shaped) and a history of heartburn” as the group most likely to benefit from screening for Barrett's esophagus. Updated practice guidelines from ACG, expected this year, may recommend screening for that population.
“The classical thinking that heartburn is going to lead you to finding Barrett's may not be true in everybody,” said Sidney Cohen, FACP, professor of medicine and gastroenterology at Thomas Jefferson University Hospital in Philadelphia.
Dr. Cohen's recent research has shown that patients found to have Barrett's esophagus do not generally report a dramatic history of reflux at the time of screening. Since the columnar mucosa that characterizes Barrett's “doesn't respond that dramatically to acid,” he said, “at the time we are seeing our patients we do not find they are having prominent reflux symptoms” and may not have had such symptoms for the preceding two or three years.
John Marshall, MD, professor of medicine in the division of gastroenterology at the University of Missouri School of Medicine, noted that the evidence does not justify widespread screening. He and many other experts worry that current guidelines encourage physicians to order unnecessary endoscopies due to potential liability concerns if they do not follow published practice guidelines.
Once Barrett's esophagus is found, the controversies continue. Determining which patients with Barrett's are going to develop esophageal cancer and how quickly is unknown, which means current recommendations about surveillance are also in flux.
The 2002 guidelines recommend that patients with Barrett's but no dysplasia undergo a repeat endoscopy in a year and then be put on a three-year cycle of checks. Those with low-grade dysplasia should be rechecked every year and those with high-grade dysplasia need to be watched every three months.
Particularly for patients with no dysplasia, “We need to reassess this,” Dr. Marshall said. “That is a lot of endoscopies but there isn't a lot of evidence supporting it.” The overall risk of a patient developing esophageal cancer if he has Barrett's but no dysplasia is about 2%, Dr. Marshall said. This compares to risks of 7% for patients with low-grade dysplasia and 22% if there is high-grade dysplasia.
“Some say that we should screen once, and if the patient doesn't have dysplasia, never look again,” explained Kenneth K. Wang, MD, professor of medicine at the Mayo Clinic and director of its Barrett's esophagus research. “The trouble is that right now, we rely on dysplasia, which is a histological marker, and histology is very inaccurate. It depends on what you sample, and it depends on the pathologist.”
Studies have proven what many physicians note anecdotally, he said: “It is very hard for pathologists to agree on what's dysplastic and what isn't.”
At some point in the future, researchers may be able to identify which precancerous cells are most likely to become cancerous by, for example, identifying cell markers in DNA. Researchers are also looking at how to take better biopsy samples to help pathologists identify dysplasia. Promising techniques being explored include using magnifiers and other optical technologies during endoscopy to target the site of the biopsy.
Treatment options
The growing incidence of Barrett's esophagus may be fueled, in part, by doctors' tendency to prescribe antacids only intermittently, said Dr. Cohen. Patients prescribed only an 8-12 week course of medication, a common practice, will relapse “virtually 100% of the time,” he observed.
Some studies have shown that an esophagus allowed to heal in a somewhat acid medium will result in Barrett's tissue growth, while healing in a non-acid environment leads to squamous cells, Dr. Cohen said. He recommended that internists put patients on lifelong maintenance doses of PPIs and refrain from recommending H2 blocker-type antacids for patients with persistent heartburn. These drugs do provide symptom relief, he said, but not effective healing.
A large research project may shed more light on whether standard treatments are effective in preventing cancer. The Aspirin Esomeprazole Chemoprevention Study (AspECT) is a multicenter, four-arm, 10-year randomized controlled clinical that will examine whether high- or low-dose esomeprazole (the PPI Nexium) and/or low-dose aspirin may be effective in preventing Barrett's metaplasia from progressing to adenocarcinoma.
Esophagectomy often is recommended for Barrett's esophagus patients with high-grade dysplasia but since esophagectomy is a difficult operation with high levels of morbidity and even mortality, experts are experimenting with all sorts of alternatives. These involve different endoscopic techniques for ablating or resecting the Barrett's mucosal lining. Dr. Wang's group at Mayo, for instance, has been working with photodynamic therapy.
“Doing any of these isn't easy, and if you have really good surgery available, that may be the better option, and if you have really good endoscopic treatment available, that may be the option,” Dr. Wang advised.
Endoscopic treatments are fraught with their own complications, including stricture formation that can affect swallowing and scarring that can complicate future follow-up, he continued. The forthcoming ACG guidelines, he said, are expected to say that endoscopic ablative therapy is a reasonable option.
For now, there is scant long-term evidence on the results of existing treatment options, said Stuart Spechler, MD, chief of gastroenterology at the Dallas VA Medical Center and professor at the University of Texas Southwestern Medical Center in Dallas. “And without [long-term data], it's hard to know that you actually cured the patient” or delayed progression to cancer.
“I would like to say that we're doing a great job, but I think we have a long way to go,” said Dr. Marshall. “Although we know a lot more about Barrett's than we used to, it just goes to show you we still have a lot more to learn.”